Open Access | Research article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Hip involvement negatively impacts postoperative radiographic outcomes after lumbar pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis—a retrospective study
#The authors contributed equally to this work.
*Corresponding author: Segni Kejela
Mailing address: The First Afliated Hospital of USTC, Division of
Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230001, P.R. China.
Email: zwzfp@163.com
Received: 29 November 2019 Accepted: 19 December 2019
DOI: 10.31491/CSRC.2019.12.042
Abstract
Background: Lumbar pedicle subtraction osteotomy (PSO) can significantly correct thoracolumbar kyphosis and relieve compensatory backward pelvic tilt (PT). However, hip involvement for some advanced ankylosing spondylitis (AS) patients can restrict the rotation of the pelvis around the femoral heads, which may affect the postoperative radiographic outcomes after lumbar PSO.
Objective To identify whether hip involvement negatively impacts the postoperative radiographic outcomes after lumbar PSO in AS patients with thoracolumbar kyphosis.
Methods: Between March 2009 and June 2013, a total of 44 consecutive AS patients with thoracolumbar kyphosis who had undergone one-level lumbar PSO were retrospectively reviewed. All the patients had more than two years of follow-up. Hip involvement was evaluated based on the Bath Ankylosing Spondylitis Radiology Hip Index (BASRI-hip) and defined by a score of at least 2. All patients were divided into group A (patients without hip involvement) and group B (patients with hip involvement). Radiographical measurements included sagittal vertical axis (SVA), global kyphosis (GK), thoracic kyphosis (TK), local kyphosis (LK), lumbar lordosis (LL), pelvic incidence (PI), PT, and sacral slope (SS). The visual analogue pain scale for low back pain was also recorded.
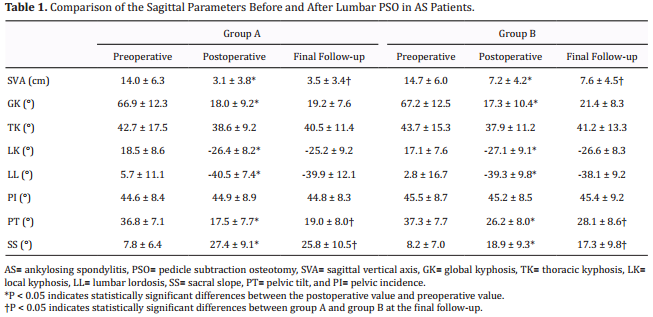
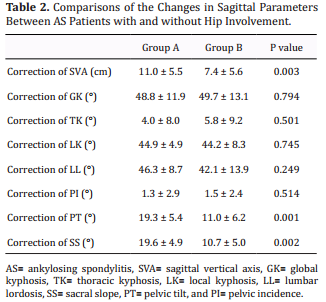
Results: Preoperative SVA and PT were not significantly different between group A and group B (SVA: 14.0 ± 6.3 cm vs. 14.7 ± 6.0 cm, P > 0.05; PT: 36.8° ± 7.1° vs. 37.3° ± 7.7°, P > 0.05), and both groups had similar magnitudes of kyphosis corrections (LK correction: 44.9° ± 4.9° vs. 44.2° ± 8.3°, P > 0.05). However, group B had significantly larger SVA and PT than group A (SVA: 7.6 ± 4.5 cm vs 3.5 ± 3.4 cm, P < 0.05; PT: 28.1° ± 8.6° vs. 19.0° ± 8.0°, P < 0.05) at the last follow-up.
Conclusion: In AS patients with thoracolumbar kyphosis, hip involvement led to insufficient correction of SVA and PT after lumbar PSO, which negatively impacted postoperative radiographic outcomes. For these patients, additional osteotomies are recommended for satisfactory correction outcomes.
Keywords
Ankylosing spondylitis; thoracolumbar kyphosis; pedicle subtraction osteotomy; hip involvement
Introduction
Ankylosing spondylitis (AS) is a chronic, progressive rheumatic disease that affects the sacroiliac joints,
spine, and peripheral joints, causing characteristic
inflammatory back pain, which can lead to structural
and functional impairments and a decrease in quality
of life [1,2]. The prevalence of AS is 0.1–1.4% globally
and 0.3% in China [1,3]. In advanced stages, more than
30% of AS patients experience thoracolumbar kyphosis, resulting in sagittal imbalance and an inability to
look straight ahead [4,5]. In an attempt to compensate
for sagittal imbalance, AS patients retrovert the pelvis
to a more vertical position and tilt the trunk backwards. This position is biomechanically inefficient and
can impair walking ability and interpersonal communication [6]. Surgical intervention is usually required
in AS patients with severe thoracolumbar kyphosis,
sagittal imbalance, and low back pain [7].
Lumbar pedicle subtraction osteotomy (PSO) is a vertebral wedge osteotomy for the correction of thoracolumbar kyphotic deformities in patients with AS and
was first described by Thomasen in 1985 [8]. In PSO,
both of the pedicles and a V-shaped bony wedge of the
vertebral body are resected. The posterior column is
shortened without lengthening the anterior column[9].
Lumbar PSO can significantly correct thoracolumbar
kyphosis, relieve compensatory backward pelvic tilt
(PT), and reconstruct the sagittal spinopelvic alignment in AS patients. Ruf et al [10]. asserted that the
corrective surgery in AS patients with thoracolumbar
kyphosis is performed to normalize PT and the gravity line and to restore the ergonomic upright position
of the body. Debarge et al. [4] claimed that the reduction of PT is one of the most common surgical targets
and that PT should be reduced to 20° to restore pelvic
orientation.
According to reports, peripheral joint disease is frequently observed in AS patients and the incidence of
hip involvement in AS patients is between 30% and
50% [11-13] Li et al. [12] found that AS patients with severe hip involvement had less range of motion during
flexion-extension, abduction-adduction, and rotation.
Hip involvement can result in decreased range of motion in the hips, which can in turn affect the rotation
of the pelvis around the femoral heads and negatively
impact postoperative radiographic outcomes. Thus,
the current study aimed to investigate whether hip
involvement can negatively impact radiographic outcomes after lumbar PSO in AS patients with thoracolumbar kyphosis.
Subjects and Methods
Subject
This study retrospectively reviewed a total of 92 consecutive AS patients who had undergone one-level
lumbar PSO for the correction of thoracolumbar kyphosis between October 2009 and October 2013. Following this, 44 AS patients (40 males and 4 females)
with a mean age of 34.8 years (range, 18–50 years)
were selected according to the study’s inclusion and
exclusion criteria. Hip involvement was assessed by
the Bath Ankylosing Spondylitis Radiology Hip Index
(BASRI-hip) scoring system and defined by a score of
at least 2 [14]. The patients were divided into group A
(patients without hip involvement) and group B (patients with hip involvement). This study was approved
by the ethics committee of the first affiliated hospital
of University of Science and Technology of China.
Inclusion criteria: The study included patients with
fixed thoracolumbar kyphosis of more than 40° [4], patients who had undergone one-level PSO at the lumbar spine, patients receiving preoperative and postoperative standing radiographs of the spine, and patients
with a minimum of two years of follow-up.
Exclusion criteria: The study excluded patients with a
preoperative coronal curve of more than 10°, patients
who had undergone previous spinal surgery, patients
who had undergone previous total hip replacement,
and patients with spinal fractures or pathological pseudarthrosis. In total, 48 AS patients were excluded from
this study (without two-year follow-up: 15 patients;
coronal curve of > 10°: 13 patients; previous spinal or
hip surgery: 8 patients; pathological spinal fractures or
pseudarthrosis: 12 patients).
Operative Procedures
Under general anesthesia, patients were placed in a prone position on a bow-type frame with the abdomen free of pressure. A standard posterior approach was used to laterally expose the posterior elements to the transverse processes. Pedicle screws were inserted 4 levels above and 3 levels below the intended osteotomy level [15,16]. Subsequently, the laminae and the articular processes of the planned osteotomy vertebra were resected and a partial laminectomy was performed at the adjacent level. Afterwards, the bilateral pedicles, dura, and bilateral nerve roots were exposed. To prevent translation and displacement, a unilateral, temporary short rod was fixed upon the pedicle screws opposite the osteotomy side. The dura and nerve root were retracted and protected with a nerve retractor. A hole was then drilled down through the pedicle into the vertebral body on the osteotomized side. The cancellous bone within the vertebral body was removed bilaterally with curettes and rongeurs. Subsequently, the posterior wall of the osteotomized vertebra was pushed down into the wedge-shaped cavity with a curette. Under direct vision of the dura and nerve roots, the osteotomy closure was carried out with the anterior cortex acting as a hinge. In the process of osteotomy closure, the bow-type frame was gradually straightened. Importantly, prior to closure of the osteotomy site, care was taken to ensure that the dural sac and nerve roots were not constricted. Finally, the temporary rod was replaced by a permanent long rod to fix the spine in the corrected position. Intraoperative neuromuscular monitoring for sensory-evoked potential and motor-evoked potential was continuously monitored during operation. All patients underwent the intraoperative wake-up test after completing instrumentation.
Radiographical Parameters
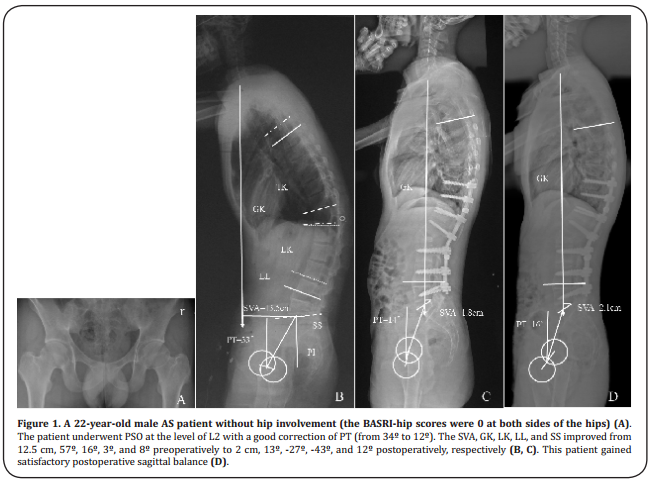
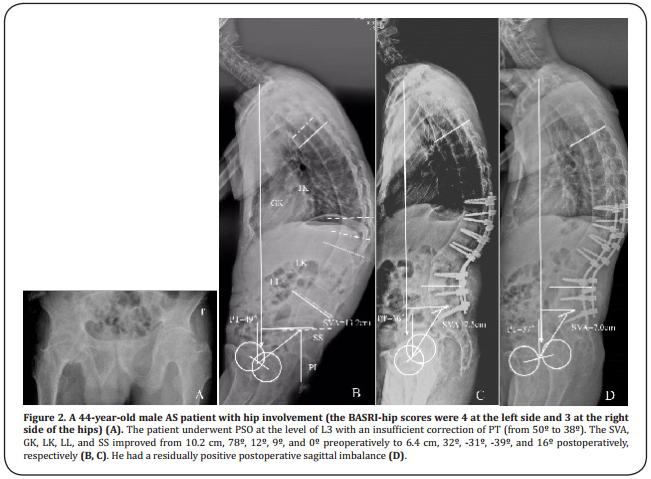
The following radiographical parameters were preoperatively and postoperatively measured on standard standing lateral radiographs of the entire spine using the Surgimap software (Spine Software, version 1.1.2, New York, NY, USA) (Figure 1, 2): (1) sagittal vertical axis (SVA) [7], defined as the distance between a plumb line dropped from the center of the seventh cervical vertebra (C7) body to the posterior-superior corner of the first sacral vertebra (S1) (the SVA was positive if the plumb line was anterior to the posterosuperior corner of S1 and negative if the plumb line was posterior to the posterosuperior corner of S1); (2) global kyphosis (GK) [7], measured as the angle formed by the upper endplate of the most cranially-tilted vertebra and the lower endplate of the most caudally-tilted vertebra; (3) thoracic kyphosis (TK) [16], calculated as the angle between the upper endplate of the the fifth thoracic vertebra (T5) vertebra and the lower endplate of the twelfth thoracic vertebra (T12); (4) local kyphosis (LK) [7], the angle between the upper endplate of the first cephalad vertebra to the osteotomy level and the lower endplate of the first caudal vertebra to the osteotomy level; (5) lumbar lordosis (LL) [4], the angle between the superior endplate of T12 and the superior endplate of S1 (the angle was positive when the curve was kyphotic and negative when the curve was lordotic); (6) pelvic incidence (PI) [17], assessed as the angle formed by the line perpendicular to the sacral plate at its midpoint and the line connecting the point to the middle axis of the femoral heads; (7) PT [17], computed as the angle formed by the vertical line and the line connecting the midpoint of the sacral plate to the middle axis of the femoral heads; and (8), sacral slope (SS) [17], the angle between the sacral plate and the horizontal line. Whereas a postoperative SVA value of 5.0 cm or less was defined as a satisfactory correction outcome, a postoperative SVA value of more than 5.0 cm was considered to indicate residual sagittal imbalance. The age, sex, and duration of the disease were also recorded in this study. An independent observer performed the measurements of all parameters. Each parameter was measured three times, and the average values were calculated in both groups.
Evaluation of low back pain improvement
The visual analogue pain scale (VAS) was used to evaluate the low back pain of the patients before and two years after surgery.
Statistical analysis
Statistical analyses were performed using SPSS statistical software, version 16.0 (SPSS Inc., Chicago, IL, USA). The sagittal parameters after the operation and at the last follow-up were compared with those before the operation by the paired-samples t test. Student’s t-tests were used to evaluate the differences in the sagittal parameters between the two groups before the surgery and at the last follow-up. Significance was defined as P < 0.05.
Results
A total of 44 AS patients (40 males and 4 females) with
a mean age of 34.8 ± 6.8 years (range, 18–50 years)
met the aforementioned inclusion criteria. The average
disease duration was 12.8 ± 6.3 years (range, 6–18
years), and the mean follow-up period was 32.4 moths
(range, 24–60 moths). None of the participants had
missing data for each variable of interest. According to
the BASRI-hip scoring system, 21 AS patients without
hip involvement were divided into group A and 23 AS
patients with hip involvement were divided into group
B. Group A was composed of 2 females and 21 males
with an average age of 33.2 ± 6.5 years (range, 18–48
years), and group B consisted of 2 females and 19
males with a mean age of 36.4 ± 7.2 years (range, 20–
50 years). The mean disease duration of AS was 12.3
± 5.3 years (range, 6–16 years) in group A and 13.4 ±
6.4 years (range, 8–18 years) in group B. The VAS for
low back pain was 6.8 in group A and 7.0 in group B.
No significant differences were found between group A
and group B for age, sex distribution, disease duration,
and VAS for low back pain (P > 0.05).
The lumbar PSO procedure was performed at the first
lumbar vertebra in 14 patients, at the second lumbar
vertebra in 24 patients, and at the third lumbar vertebra in 6 patients. No intraoperative or postoperative
neurovascular complications were observed in all
cases. Sagittal subluxation of osteotomized vertebra
occurred in one patient without neurological deficits. Wound infection was found in two patients, and
the wounds healed well when the patients were discharged. The infection rate for the current study was
about 4.5%. Dural tear occurred in two patients when
the ossified ligamentum flavum was dissected from
the dura. With the prompt intraoperative management
of the leaks with gel sponges, the patients recovered
without adverse effects by the time of their final follow-ups.
Discussion
During advanced stages, more than 30% of AS patients
experience thoracolumbar kyphosis [1,4]. With the progression of the disease, severe thoracolumbar kyphosis can lead to sagittal imbalance and the inability to
look straight ahead [18,19]. In order to maintain an erect
posture, AS patients retrovert the pelvis to a more vertical position and tilt the entire rigid segment of the
spine backwards [5]. This posture does not completely
compensate for their sagittal imbalance, which dramatically restricts their daily activities and decreases
their quality of life [18]. Therefore, reconstructive procedures are recommended to correct sagittal imbalance and to restore the ability for AS patients to look
straight ahead [5].
Lumbar PSO has been widely used to correct AS-related thoracolumbar kyphosis, restore backward PT, and
reconstruct sagittal spinopelvic balance [16]. Song et al.
[20] studied 20 AS patients who had undergone spinal
osteotomies to correct their kyphotic deformities. The
study’s results showed that GK, PT, and SVA were significantly corrected from 53°, 30°, and 18 cm preoperatively to 3°, 11°, and 7 cm postoperatively. However,
hip involvement was found in 30% to 50% of advanced
AS patients, which can decrease the range of motion of
the hips and affect the rotation of the pelvis around the
femoral heads [11]. Until now, few studies have focused
on whether hip involvement can negatively impact
postoperative radiographic outcomes after lumbar PSO
in AS patients.
Several previous studies have reported that highly-retroverted pelvises in AS patients can be corrected by
lumbar PSO with the realignment of the spine [7,12]. In
Qian et al.’s [7] analyses of the sagittal spinopelvic parameters of 36 AS patients who had undergone lumbar
PSO, they found that PT could be restored from 35.9°
± 7.3° preoperatively to 22.3° ± 7.9° postoperatively
with the correction of GK from 73.7° ± 16.5° to 25.3° ±
11.7°. The results demonstrated that the PSO-induced
correction of the thoracolumbar kyphosis relieved the
compensatory backward PT. Chen et al. [22] asserted
that structural damage to the hips can contribute to
mobility limitation, functional impairment, and the inability to exercise. Rousseau et al. [23]studied the spinal
balance of 356 patients and determined that spondylarthritis cases showed less pelvic reorientation after
lumbar PSO, probably due to limitations in hip mobility.
In the present study, the correction of PT was smaller
in group B than in group A (11.0° ± 6.2° vs. 19.3° ± 5.4°) and the postoperative PT was significantly larger in
group B than in group A (26.2° ± 8.0° vs. 17.5° ± 7.7°,
P < 0.05) (Figures 1, 2). Thus, we deemed that hip involvement affected the rotation of the pelvis around
the femoral heads, leading to the insufficient correction of PT after lumbar PSO. In addition, because the
pelvis acts as an intercalary unit between the spine and
the lower extremities, the position of the pelvis plays
a critical role in maintaining standing postures. Lee et
al. [18] observed that PT was a significant parameter in
determining sagittal balance in AS patients. Debarge
et al. [4] ascertained that sagittal balance cannot be sufficiently corrected with a h0igh PT after lumbar PSO.
Similarly, in the current study, the postoperative SVA
was found to be significantly larger in group B than in
group A (7.2 ± 4.2 cm vs. 3.1 ± 3.8 cm, P < 0.05) (Figures
1 and 2). Therefore, we concluded that hip involvement in AS patients limited the range of motion in hips,
leading to the insufficient correction of PT and SVA and
impacting postoperative radiographic outcomes after
lumbar PSO.
This study contains two limitations that need to be addressed. First, because it did not perform assessments
of hip range of motion, it was unable to establish a
relationship between the correction of PT and hip
range of motion. Second, as the study did not analyze
the influence of osteotomy levels on the degree of PT
correction in AS patients, this factor should be a point
of focus in future research. In spite of these limiting
factors, this study was the first of its kind to investigate
how hip involvement negatively impacts postoperative
radiographic outcomes after lumbar PSO in AS patients.
Conclusion
The results of this study demonstrate for the first time that hip involvement can lead to insufficient SVA and PT correction and negatively impact postoperative radiographic outcomes in AS patients with thoracolumbar kyphosis. Therefore, for AS patients with thoracolumbar kyphosis who require lumbar PSO surgery, the preoperative assessment of hip involvement plays a pivotal role. For AS patients with both spine and hip deformities, additional osteotomies may be recommended for satisfactory correction outcomes.
Declaration
Conflicts of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Funding
This article is supported by the Fundamental Research Funds for the Central Universities (WK9110000083).
References
1. Braun, J., & Sieper, J. (2007). Ankylosing spondylitis. The
Lancet, 369(9570), 1379-1390.
2. Qian, B. P., Jiang, J., Qiu, Y., Wang, B., Yu, Y., & Zhu, Z. Z.
(2014). The presence of a negative sacral slope in patients
with ankylosing spondylitis with severe thoracolumbar
kyphosis. JBJS, 96(22), e188.
3. Liu, Y., Li, L., Shi, S., Chen, X., Gao, J., Zhu, M., & Yuan, J.
(2016). Association study of ankylosing spondylitis and
polymorphisms in ERAP1 gene in Zhejiang Han Chinese
population. Rheumatology international, 36(2), 243-248.
4. Debarge, R., Demey, G., & Roussouly, P. (2010). Radiological analysis of ankylosing spondylitis patients with severe
kyphosis before and after pedicle subtraction osteotomy. European Spine Journal, 19(1), 65-70.
5. Kim, K. T., Lee, S. H., Suk, K. S., Lee, J. H., & Jeong, B. O. (2012).
Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine, 37(19), 1667-1675.
6. Shin, J. K., Lee, J. S., Goh, T. S., & Son, S. M. (2014). Correlation
between clinical outcome and spinopelvic parameters in
ankylosing spondylitis. European Spine Journal, 23(1),
242-247.
7. Qian, B. P., Jiang, J., Qiu, Y., Wang, B., Yu, Y., & Zhu, Z. Z.
(2013). Radiographical predictors for postoperative sagittal imbalance in patients with thoracolumbar kyphosis
secondary to ankylosing spondylitis after lumbar pedicle
subtraction osteotomy. Spine, 38(26), E1669-E1675.
8. Thomasen, E. I. V. I. N. D. (1985). Vertebral osteotomy for
correction of kyphosis in ankylosing spondylitis. Clinical
orthopaedics and related research, (194), 142-152.
9. Qian, B. P., Qiu, Y., Wang, B., Sun, X., Zhu, Z. Z., Jiang, J., &
Ji, M. L. (2012). Pedicle subtraction osteotomy through
pseudarthrosis to correct thoracolumbar kyphotic deformity in advanced ankylosing spondylitis. European spine
journal, 21(4), 711-718.
10. Ruf, M., Wagner, R., Merk, H., & Harms, J. (2006). Preoperative planning and computer assisted surgery in ankylosing spondylitis. Zeitschrift fur Orthopadie und ihre
Grenzgebiete, 144(1), 52-57.
11. Joshi, A. B., Markovic, L., Hardinge, K., & Murphy, J. C.
(2002). Total hip arthroplasty in ankylosing spondylitis:
an analysis of 181 hips. The Journal of arthroplasty, 17(4),
427-433.
12. Li, J., Xu, W., Xu, L., & Liang, Z. (2009). Hip resurfacing
arthroplasty for ankylosing spondylitis. The Journal of
arthroplasty, 24(8), 1285-1291.
13. Tang, W. M., & Chiu, K. Y. (2000). Primary total hip arthroplasty in patients with ankylosing spondylitis. The Journal
of arthroplasty, 15(1), 52-58.
14. MacKay, K., Brophy, S., Mack, C., Doran, M., & Calin, A.
(2000). The development and validation of a radiographic grading system for the hip in ankylosing spondylitis:
the bath ankylosing spondylitis radiology hip index. The
Journal of rheumatology, 27(12), 2866-2872.
15. Chen, H., Chien, J. T., & Yu, T. C. (2001). Transpedicular
wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine, 26(16), E354-E360.
16. Qian, B. P., Wang, X. H., Qiu, Y., Wang, B., Zhu, Z. Z., Jiang, J.,
& Sun, X. (2012). The influence of closing-opening wedge
osteotomy on sagittal balance in thoracolumbar kyphosis
secondary to ankylosing spondylitis: a comparison with
closing wedge osteotomy. Spine, 37(16), 1415-1423.
17. Le Huec, J. C., Aunoble, S., Philippe, L., & Nicolas, P. (2011).
Pelvic parameters: origin and significance. European
Spine Journal, 20(5), 564.
18. Lee, J. S., Suh, K. T., Kim, J. I., & Goh, T. S. (2014). Analysis of
sagittal balance of ankylosing spondylitis using spinopelvic parameters. Clinical Spine Surgery, 27(3), E94-E98.
19. Wang, Y., Zhang, Y., Mao, K., Zhang, X., Wang, Z., Zheng, G.,
Wood, K. B. (2010). Transpedicular bivertebrae wedge osteotomy and discectomy in lumbar spine for severe ankyWen-zhi Zhang et al 37
losing spondylitis. Clinical Spine Surgery, 23(3), 186-191.
20. Song, K., Zheng, G., Zhang, Y., Zhang, X., Mao, K., & Wang,
Y. (2013). A new method for calculating the exact angle
required for spinal osteotomy. Spine, 38(10), E616-E620.
21. Kiaer, T., & Gehrchen, M. (2010). Transpedicular closed
wedge osteotomy in ankylosing spondylitis: results of surgical treatment and prospective outcome analysis. European Spine Journal, 19(1), 57-64.
22. Chen, H. A. , Chen, C. H. , Liao, H. T. , Lin, Y. J. , Chen, P.
C. , & Chen, W. S. , et al. (2011). Factors associated with
radiographic spinal involvement and hip involvement in
ankylosing spondylitis. Seminars in Arthritis & Rheumatism, 40(6), 552-558.
23. Rousseau, M. A., Lazennec, J. Y., Tassin, J. L., Fort, D., & la
Scoliose, G. D. E. (2014). Sagittal rebalancing of the pelvis
and the thoracic spine after pedicle subtraction osteotomy
at the lumbar level. Clinical Spine Surgery, 27(3), 166-173.