Open Access | Research article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
X-ray measurement and analysis on parameters of intervertebral foramen in the lower lumbar spine associated with the superior articular process
*Corresponding author: Yang Yu
Mailing address: Department of bone and spine surgery, Jinzhou
medical university, Jinzhou, China.
Email: doctoryoung@163.com
Received: 18 January 2020 Accepted: 09 April 2020
DOI: 10.31491/CSRC.2020.03.048
Abstract
Objectives: In this study, we aimed to supplement the database of intervertebral foramen by measuring the
parameters of the lower lumbar spine related to the articular process of the X-ray, which could lay a theoretical
foundation for the individualized surgery of transforaminal endoscopic spine technique (TEST).
Methods: Anteroposterior and lateral X-rays of the lumbar spine from 104 adults (50 male and 54 female) who
met the measurement criteria were selected. The height and width of the intervertebral foramen, the height of
the intervertebral space, the length from the superior articular process (SAP) to the lower edge of the upper
lumbar pedicle, and the length from SAP to posterior margin of superior vertebra posterior edge were measured.
Results: There was no significant difference in the shape of the lower lumbar intervertebral foramen between
normal adult men and women. There were significant differences in parameters related to the lower lumbar
intervertebral foramen between the age group from 40 to 60 and above 60, and especially those related to the
SAP.
Conclusion: Parameters of the lower lumbar intervertebral foramen were obtained from 104 normal adults,
which supplemented the lumbar intervertebral foramen database. After the age of 60, the morphology of the
lower lumbar intervertebral foramen was significantly changed in normal adults, and especially parameters
related to the SAP. This study provided a reference for individualized minimally invasive surgery using TEST
for elderly people over 60 years of age.
Keywords
Transforaminal endoscopic spine technique; superior articular process; intervertebral foramen; lower lumbar spine; X-ray; age
Introduction
Symptomatic lumbar disc herniation (LDH) is one of the
common causes of spinal surgery. Surgical treatment has
evolved from traditional spine surgery to transforaminal percutaneous endoscopic discectomy (TPED) using
the transforaminal endoscopic spine technique (TEST) [1]. TEST has several advantages such as less trauma, faster recovery, less scarring and more complete retention
of the original physiological structure of the spine. And
research showed that there was no statistical difference
in clinical efficacy between spinal endoscopy and traditional open spinal surgery [2].
A large number of present studies have reported that
TEST is a successful system operation, and the inserted
cannula by transforaminal spinal endoscopy can safely
pass through the intervertebral foramen [3-6]. With the
emergence of the transforaminal technique, the importance of the study on the intervertebral foraminal morphology is self-evident, which has led to more research on
the morphological characteristics of the intervertebral
foramen [7-11]. Intervertebral foraminal morphology is
particularly important for transforaminal spinal endoscopy. A natural hole composed of two adjacent vertebral
pedicles contains nerves and blood vessels. The upper
and lower boundaries are the upper vertebral vertebrae.
Roof and floor are formed by inferior and superior notch
of respective vertebral pedicles. The anterior boundary
is composed of two vertebral discs and the posterior
longitudinal ligament, and the posterior boundary is
composed of the capsule of the small joint and part of
the yellow ligament [12]. The shape of the intervertebral foramen is not constant, and some pathological changes
will cause the morphologic change of the intervertebral
foramen [13]. Many studies showed that the movement of
the lumbar spine can also change of the morphology of
the intervertebral foramen [14-16]. The study of intervertebral foraminal morphology has guiding significance
for the imaging diagnosis and treatment of lumbar spine
diseases. In terms of the technique of transforaminal
spinal endoscopy, it is of guiding significance to grasp
the parameters of intervertebral foramina for accurate
insertion of cannula [17].
The superior articular process (SAP) is an important
part of the intervertebral foramen, and the morphology of the SAP is also an influencing important factor of
intervertebral foramen stenosis and the nerve root compression. Intervertebral foramen stenosis was related
to the degeneration of the intervertebral space and the
upward movement of the SAP: the height of intervertebral space decreased, resulting in the height of intervertebral foramen reduced. The osteophyte formation of
the articular process and the thickened of the ligament
flava lead to the intervertebral foramen stenosis [7-11].
Hoogland et al. in 2006 proposed the transforaminal
endoscopic spine system (TESSYS) technology, which
is quite representative of TEST. The surgical procedure
requires the use of a ring drill to grind the SAP in order
to successfully place the cannula into the spinal canal indicating that the morphology of the SAP is an important
factor for whether the cannula can enter the spinal canal
in TESSYS technology. However, only a limited number
of studies have included the intervertebral foramen, and
even less has been done on the measurement of parameters associated with the SAP. In order to better grasp
the geometry of the intervertebral foramen and improve
the success rate of surgery, this study supplemented the
database of the intervertebral foramen by measuring
the parameters of the lower lumbar vertebra related to
the SAP of the X-ray, which could provide a reference for
the individualized surgery of TEST.
Methods and materials
General information
104 adults (50 male and 54 female) were selected from
the outpatient and inpatient cases in the first affiliated
hospital of Jinzhou Medical University who were to receive anteroposterior and lateral X-ray photographs of
the lumbar spine from October 2017 to May 2019, all of
whom were aged from 18 to 80. Male age: 50.65±14.52,
female age: 49.63±18.04.
Inclusion criteria:(1) No history of lumbar disease and
lumbar trauma;(2) No history of waist and leg pain and
lower extremity radiation pain;(3) No history of lumbar
spine fractures and surgery;(4) No nerve root symptoms
such as lower limb numbness and intermittent claudication;(5) The selected samples were taken in accordance
with unified standards. No lumbar disc herniation, no
lumbar spinal stenosis, lumbar pathological changes,
osteogenesis, lumbar spondylolisthesis, scoliosis and
other congenital or acquired osteopathy were confirmed
as normal lumbar spine by X-ray imaging examination.
Measurement methods and parameters
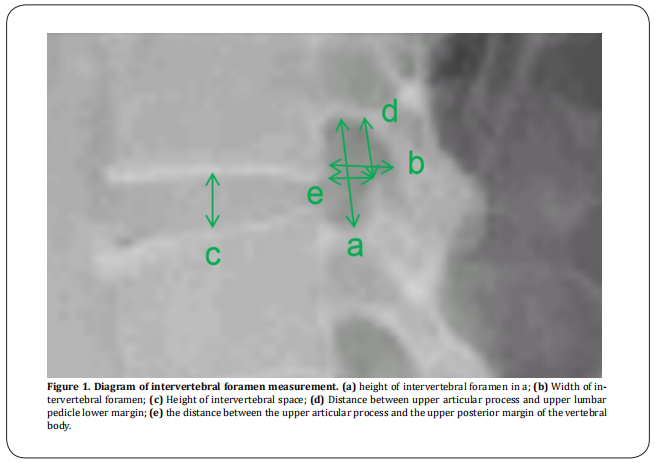
The upright and lateral positions of the lumbar spine were photographed in the standing position. The projection centre was about 3 cm above the condyle, about 8 cm before the lumbar spinous process, about L3 vertebral level, and the projection distance was about 100 cm, referring to the scale on the X-ray. The X-ray can clearly and completely show the shape of the intervertebral foramen and the SAP. The following parameters of each intervertebral foramen (l3-l4, l4-l5, l5-s1) were measured and recorded on the X-ray of the lateral lumbar spine: (1) Determine the height of the intervertebral foramen in the lower lumbar vertebra (a). Use the measurement tool on the computer imaging software to make a line between the midpoint of the upper pedicle and the midpoint of the lower pedicle and read it. The value is the height of the intervertebral foramen (a); (2) Determine the width of the intervertebral foramen in the lower lumbar vertebra (b). For the superior lumbar pedicle, record the length from the posterior cortex of the lamina to the posterior cortex of the vertebral body, which is the width of the intervertebral foramen (b); (3) Determine the height of the intervertebral foramen in the lower lumbar spine (c). The length from the lower edge of the upper vertebrae to the upper edge of the lower vertebrae is the intervertebral height value (c); (4) Determine the distance from the SAP in the lower lumbar spine to the lower edge of the upper lumbar pedicle (d). The length from the apex of the SAP in the lower lumbar spine to the lower edge of the upper lumbar pedicle is d value ;(5) Determine the distance from the SAP in the lower lumbar vertebrae to the posterior edge of the upper vertebra (e). The length from the apex of the superior articular process in the lower lumbar vertebrae to the posterior edge of the vertebral body is e value(Figure1).
Statistical analysis
The statistical software SPSS 21.0 was used for statistical analysis, and all results were represented as means ± standard deviations. The obtained data were tested for normality, and the original data met the normality requirements of anova. The independent sample t-test was used to compare the differences caused by gender and age. When P < 0.05, the differences were considered statistically significant.
Results
X-ray measurement of the lower lumbar intervertebral foramen in normal adults
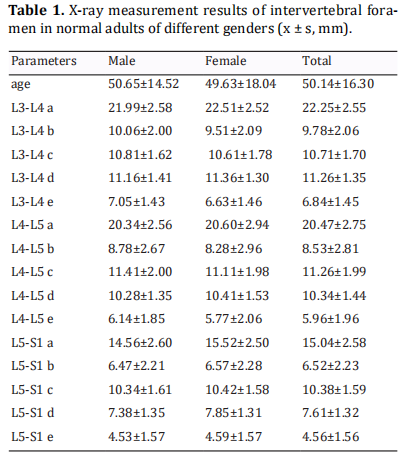
A total of 300 lumbar X-rays (L3/4, L4/5, L5/S1) in 104 normal adults were measured and analyzed. The obtained data were all counting data, which were consistent with normal distribution by normal test. The relevant parameters of the lower lumbar foramen in normal adults were successively as follows: the heights of the intervertebral foramen were 22.25±2.55mm, 20.47±2.75mm, and 15.04±2.58mm; The widths of the intervertebral foramen were 9.78±2.06mm, 8.53±2.81mm, and 6.52±2.23mm; The heights of the lumbar intervertebral were 10.71±1.70mm, 11.26±1.99mm, and 10.38±1.59mm; The lengths from SAP to the lower edge of the upper lumbar pedicle were 11.26±1.35mm, 10.34±1.44mm, and 7.61±1.32mm; The lengths from SAP to posterior margin of superior vertebra posterior edge were 6.84±1.45mm, 5.96±1.96mm, 4.56±1.56mm.
Parameters of the intervertebral foramen in the lower lumbar spine of different genders
The measured data of various parameters in the lower lumbar intervertebral foramen between different genders were shown in Table 1. The results showed that there was no significant difference in the parameters of the lower lumbar intervertebral foramen between different genders (P>0.05).
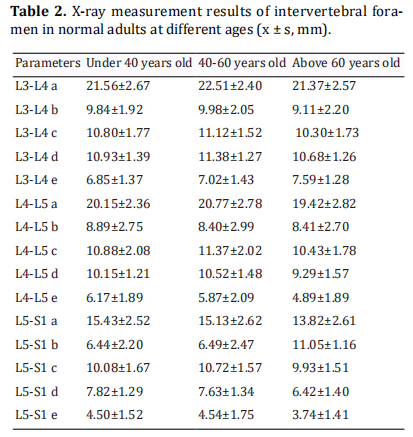
Parameters of the intervertebral foramen in the lower lumbar spine at different ages
The data of male and female groups were combined and counted, and a total of 104 cases were divided into three groups according to age: 28 cases under 40 years old, 41 cases between 40 and 60 years old, and 35 cases above 60 years old. A statistical comparison of the parameters in the lower lumbar intervertebral foramen among the three groups showed that there was a difference between the age group under 40 and the age group between 40 and 60, but the difference was not statistically significant. There were significant differences in parameters a, c, d and e between the age group from 40 to 60 years old and the age group above 60 years old (Table 2). Meanwhile, it was found that the differences in parameters related to the SAP were particularly significant, and the differences were statistically significant (p<0.05).
Discussion
Our results suggested that there were no significant
differences between parameters in the lower lumbar
intervertebral foramen between normal males and females. Gkasdaris G et al. found that no significant width
differences for intervertebral foramen was observed at
any level for either sex whether measured directly from
the body or by CT [18,19]. This finding was also consistent
with earlier reports on the sex-dependent size of the
spinal dimension [20,21].
There were differences in parameters a, c, d, and e between the age group from 40 to 60 years old and the age
above 60 years old. Adams and Hutton [22] found that the
intervertebral joints were subjected to different stresses
in different positions, and the lower the intervertebral
space height, the more stress on the superior articular
process, and the elder‘s lumbar superior articular process receives more stress than the youngers'. According
to ‘Wolf's Law’ [23], bone is not an invariable material.
It has the ability to reshape and repair after repeated
damage under chronic external pressure for a long time
in order to better adapt to the environment. As time goes
on, these small changes gradually affect the anatomical
structure of bones, ultimately leading to people over 60
show significant differences in intervertebral foramen
parameters compared to those under 60. With the improvement of living standards, the aging of China and
the world's population will be inevitable. Therefore,
our data could have clinical application on individualized minimally invasive surgery using transforaminal
endoscopic spine technique for elderly people over 60
years of age. Our results also suggested that parameters
related to the superior articular processes change more
significantly. Many studies have reported that [7-11] intervertebral foramen stenosis was related to the degeneration of the intervertebral space and upward movement of the superior articular process. The decrease of
the intervertebral space height leads to a decrease in
the height of the intervertebral foramen. The formation
and hypertrophy of the facet joint capsule lead to the
narrowing of the intervertebral foramen and compress
the corresponding nerve roots. Due to factors such as
degeneration of the intervertebral space and the movement of the articular processes, the height and width of
the intervertebral foramen vary widely between reports.
These may cause differences in the parameters of the
lower lumbar intervertebral foramen between different ages. But we speculated that the changes in the two
parameters related to the superior articular process in
our results were associated to the decrease in the height
of the intervertebral space. When the height of the intervertebral space decreased, it needs to further investigate whether the length from SAP to the lower edge
of the upper lumbar pedicle (d) is more sensitive and
representative than the intervertebral foraminal height.
This study is only a part of the regional anatomy data
obtained from the X-ray parameters of the lower lumbar
intervertebral foramen associated with the SAP, and can
merely provide a limited reference for the diagnosis and
treatment of TEST and lumbar spinal stenosis. The specific application of our data to the guidance of intervertebral foraminal endoscopic surgery needs to be further
studied and discussed.
Conclusion
Parameters of the lower lumbar intervertebral foramen were obtained from 104 normal adults, which supplemented the lumbar intervertebral foramen database. After the age of 60, the morphology of the lower lumbar intervertebral foramen was significantly changed in normal adults, and especially parameters related to the SAP. Our data could have clinical application on individualized minimally invasive surgery using TEST.
Declarations
Financial support and sponsorship
Funded by the Natural Science Foundation of Liaoning Province (No : 20180550920).
Conflicts of interest
The author declares that there is no conflict of interest.
References
1. Kapetanakis, S., Gkasdaris, G., Angoules, A. G., & Givissis,
P. (2017). Transforaminal percutaneous endoscopic
discectomy using transforaminal endoscopic spine
system technique: pitfalls that a beginner should avoid.
World journal of orthopedics, 8(12), 874.
2. Telfeian, A. E., Iprenburg, M., & Wagner, R. (2017).
Endoscopic spine surgery: distance patients will travel
for minimally invasive spine surgery. Pain physician, 20,
E145-E149.
3. Choi, I., Ahn, J. O., So, W. S., Lee, S. J., Choi, I. J., & Kim, H.
(2013). Exiting root injury in transforaminal endoscopic
discectomy: preoperative image considerations for
safety. European Spine Journal, 22(11), 2481-2487.
4. Tsou, P. M., & Yeung, A. T. (2002). Transforaminal
endoscopic decompression for radiculopathy secondary
to intracanal noncontained lumbar disc herniations:
outcome and technique. The Spine Journal, 2(1), 41-48.
5. Ruetten, S., Komp, M., Merk, H., & Godolias, G. (2008).
Full-endoscopic interlaminar and transforaminal lumbar
discectomy versus conventional microsurgical technique:
a prospective, randomized, controlled study. Spine, 33(9),
931-939.
6. Yeung, A. T., & Tsou, P. M. (2002). Posterolateral
endoscopic excision for lumbar disc herniation: surgical
technique, outcome, and complications in 307 consecutive
cases. Spine, 27(7), 722-731.
7. Min, J. H., Kang, S. H., Lee, J. B., Cho, T. H., Suh, J. K., &
Rhyu, I. J. (2005). Morphometric analysis of the working
zone for endoscopic lumbar discectomy. Clinical Spine
Surgery, 18(2), 132-135.
8. Mirkovic, S. R., Schwartz, D. G., & Glazier, K. D. (1995).
Anatomic considerations in lumbar posterolateral
percutaneous procedures. Spine, 20(18), 1965-1971.
9. Epstein, B. S., Epstein, J. A., & Lavine, L. (1964). The effect
Yang Yu et al 25
of anatomic variations in the lumbar vertebrae and spinal
canal on cauda equina and nerve root syndromes. The
American journal of roentgenology, radium therapy, and
nuclear medicine, 91, 1055.
10. Giles, L. G. (1994). A histological investigation of
human lower lumbar intervertebral canal (foramen)
dimensions. Journal of manipulative and physiological
therapeutics, 17(1), 4-14.
11. Torun, F., Dolgun, H., Tuna, H., Attar, A., Uz, A., & Erdem,
A. (2006). Morphometric analysis of the roots and
neural foramina of the lumbar vertebrae. Surgical
neurology, 66(2), 148-151.
12. Choi, G., Pophale, C. S., Patel, B., & Uniyal, P. (2017).
Endoscopic spine surgery.Journal of Korean Neurosurgical
Society, 60(5), 485.
13. Bulyshchenko, G. G., Gaivoronskii, A. I., & Gaivoronskii, I. V.
(2018). Morphoscopic and Morphometric Characteristics
of Intervertebral Foramina in the Lumbar Segment of the
Spine. Neuroscience and Behavioral Physiology, 48(5),
582-587.
14. Revel, M., Mayoux-Benhamou, M. A., Aaron, C., & Amor,
B. (1988). Variations morphologiques des trous de
conjugaison lombaires lors de la flexion-extension et de
l’affaissement discal. Rev Rhum Mal Ostéoartic, 5, 361-
366.
15. Panjabi, M. M., Takata, K. O. I. C. H. I. R. O., & Goel, V. K. (1983).
Kinematics of lumbar intervertebral foramen. Spine, 8(4),
348-357.
16. Inufusa, A., An, H. S., Lim, T. H., Hasegawa, T., Haughton,
V. M., & Nowicki, B. H. (1996). Anatomic changes of the
spinal canal and intervertebral foramen associated with
flexion-extension movement. Spine, 21(21), 2412-2420.
17. Imran, J. B., Madni, T. D., Pruitt, J. H., Cornelius, C.,
Subramanian, M., Clark, A. T., ... & Eastman, A. L. (2018).
Can CT imaging of the chest, abdomen, and pelvis identify
all vertebral injuries of the thoracolumbar spine without
dedicated reformatting?. The American Journal of
Surgery, 216(1), 52-55.
18. Gkasdaris, G., Tripsianis, G., Kotopoulos, K., & Kapetanakis,
S. (2016). Clinical anatomy and significance of the thoracic
intervertebral foramen: A cadaveric study and review
of the literature. Journal of craniovertebral junction &
spine, 7(4), 228.
19. GKASDARIS, G., HOURMOUZI, D., CHANIOTAKIS, C.,
HARITOUDIS, G., ASHRAFI, M. M., MOUSELIMIS, D., &
KAPETANAKIS, S. (2018). CT Assessment of the in vivo
Osseous Lumbar Intervertebral Foramen: a Radiologic
Study with Clinical Applications. Maedica, 13(4), 294.
20. Hasue, M., Kunogi, J. U. N. I. C. H. I., Konno, S. H. I. N. I. C. H.
I., & Kikuchi, S. (1989). Classification by position of dorsal
root ganglia in the lumbosacral region. Spine, 14(11),
1261-1264.
21. Kikuchi, S. H. I. N. I. C. H. I., Hasue, M. I. T. S. U. O., Nishiyama,
K. E. I. J. I., & Ito, T. S. U. K. A. S. A. (1984). Anatomic and clinical studies of radicular symptoms. Spine, 9(1), 23-30.
22. Adams, M. A., & Hutton, W. C. (1980). The effect of
posture on the role of the apophysial joints in resisting
intervertebral compressive forces. The Journal of bone
and joint surgery. British volume, 62(3), 358-362.
23. Wolff, J. (1893). Das gesetz der transformation
der knochen. DMW-Deutsche Medizinische
Wochenschrift, 19(47), 1222-1224.