Open Access | Case Report
This work is licensed under a
Creative Commons Attribution-ShareAlike 4.0
International License.
En-bloc excision of Giant Cell Tumors of the distal radius and arthrodesis of the translocated ipsilateral ulna: A report of two cases
* Correspondence to: Eva Campos-Pereira
Mailing address: Department of Orthopaedics, Hospital Central
do Funchal, Funchal, Portugal.
E-mail: eva.campos.pereira@gmail.com
Received: 02 September 2021 / Accepted: 15 December 2021
DOI:
10.31491/CSRC.2021.12.084
Abstract
The distal radius is the third most common site of giant cell tumor of bone (GCTB). The local aggressive invasion of this rare neoplasm requires reconstructive solutions after wide excision. The authors present two cases of patients diagnosed with Campanacci grade III GCTB of the distal radius successfully treated with en-bloc excision and translocation of the ipsilateral ulna. Pre-operative application of denosumab was given for one year to both patients. At one year of follow-up, both patients are disease-free and reported satisfactory results on Quick - Disabilities of the Arm, Shoulder and Hand (Quick-DASH) questionnaire and modified Musculoskeletal Tumor Society (MSTS) score. Although a challenge, the reported procedure offers good oncological and functional outcomes.
Keywords
Giant cell tumor of bone; distal radius; en-bloc excision; translocation; ipsilateral ulna; wrist arthrodesis
Introduction
Giant cell tumor of bone (GCTB) is a benign but locally
aggressive intramedullary bone tumor that was first
described in 1818 by Cooper and Travers [1-3]. The distal
radius is the third most common site of GCTB after
distal femur and proximal tibia [1, 4-7]. Local recurrences
occur in 70% of the cases within 24 months after excision
and lung metastasis in 2% of the patients [7-10].
Typically, local pain with an increased
swelling is
reported
and a pathological fracture occurs in 10% of the
patients because of the tumor's osteolytic nature [3, 11].
The radiological system of 3 stages described by Campanacci
et al. demonstrates a clinical-radiological cor-
Case Report
relation. In stage I, latent lesions have a well-marginated
border and do not perforate the cortical bone. Stage
II lesions are active, without a radiopaque rim or soft
tissue involvement. Stage III tumors are aggressive,
without well-defined limits, with rapid and permeated
growth, with involvement of the surrounding soft
tissue. For both stages, I and stage II lesions, intralesional
curettage and acrylic bone cement (or other
substitutes) are the most reported treatment [3-8, 10, 12-14].
Nevertheless, more aggressive
treatment
protocols are
required to prevent the recurrence of lesions at stage
III. Although adjuvant agents decrease the recurrence
rates of intralesional curettage, this primary option has
higher recurrence rates (up to 27%) than wide resection
(0 to 12%) [6, 8, 15, 16].
Denosumab, a human monoclonal antibody against
RANKL (receptor activator of nuclear factor-kB ligand),
contains tumor growth and facilitates resection without
contamination when used as neoadjuvant therapy
in aggressive lesions [1, 10].
After resection of complex lesions, surgeons must consider
the pros and cons of the different reconstructive
options already described. Despite the consensus in
radical tumor excision, the best wrist reconstructive
option is not well defined.
The authors describe two cases of patients diagnosed
with Campanacci grade III GCTB of the distal radius reconstructed
with ipsilateral ulnar autograft and wrist
fusion following en-bloc resection with good oncological
and functional results.
Case Report
Case 1
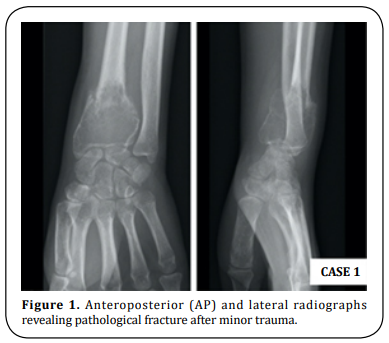
A 35-year-old right-hand dominant male presented
with a painful and enlarging mass on his left wrist,
with six months evolution. The patient referred that,
two months before mass detection, a pathological fracture was diagnosed after minor trauma (Figure
1). On physical examination the distal forearm was
tender and hypoesthesia in the ulnar nerve territory
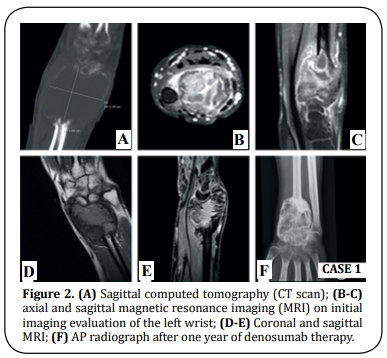
was present. Pre-operative anteroposterior and lateral
radiographs, computed tomography scan (CT scan),
and magnetic resonance imaging (MRI) revealed an
expansible lesion located within the epiphysis of the
distal radius, compatible with a Campanacci grade III
GCTB (Figure 2). He underwent a CT scan guided core
biopsy. The histological report confirmed GCTB. No
other lesions were detected in staging imaging. The patient
completed one year of neoadjuvant therapy with
denosumab (120 mg subcutaneous (SC) per 28 days,
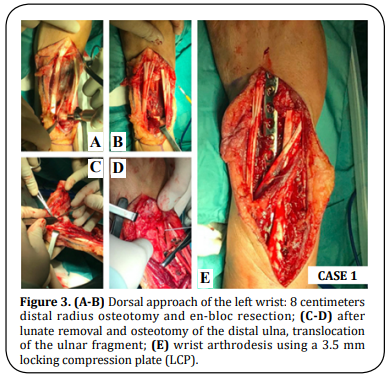
during 12 months) (Figure 2). The patient underwent
an 8 centimeters dorsal en-bloc resection of the distal
radius and an ulnar osteotomy at the same level of the
radius osteotomy, retaining muscular attachments. The
lunate was removed and the joint surface of the ulna as well as the remaining carpal bones was decorticated.
The distal ulna was transposed and aligned with the
remaining radius and the third metacarpal bone. An
uneventful fixation was performed with a dorsal 3.5
mm locking compression plate (LCP) with slight dorsiflexion
and ulnar deviation (Figure 3). The histological
report confirmed wide resection (R0).
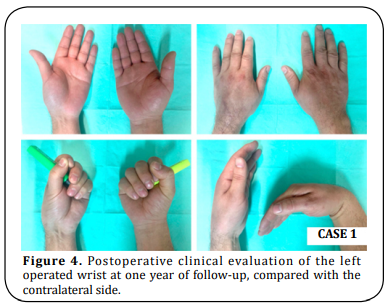
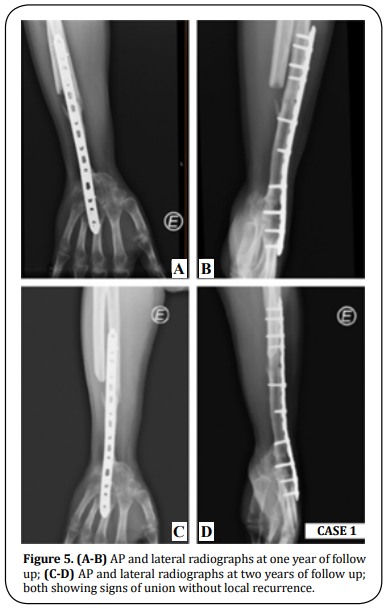
The patient was immobilized with an above-elbow cast for three weeks and a below-elbow splint for two more weeks. The patient underwent an intensive program of physiotherapy for eight months. At one year of follow-up, the patient presented full flexion/extension of the fingers and full supination/pronation (SN/PN) (Figure 4) without pain. The modified Musculoskeletal Tumor Society score (MSTS) was 21 (compared to the pre-operative value of 9) and the Quick - Disabilities of the Arm, Shoulder and Hand questionnaire (Quick- DASH) was 22,7 (compared to the pre-operative value of 88,6). The mean handgrip value, evaluated with a Jamar dynamometer, for the operated side was 51,8 Libras (lbs) compared to 93,9 lbs for the contralateral side. Radiographs showed bone fusion at both ends of the ulna and discarded local recurrence at two years of follow-up (Figure 5).
Case 2
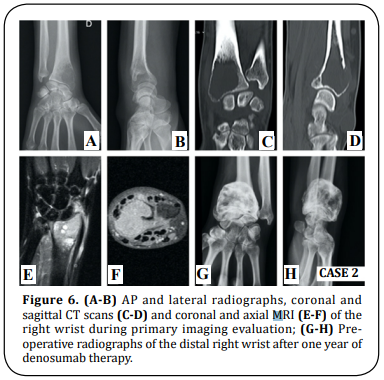
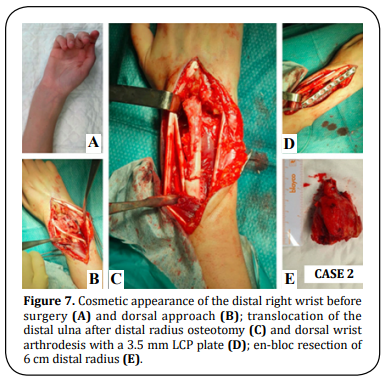
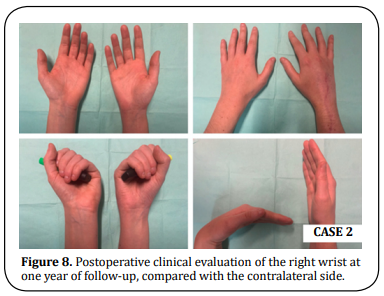
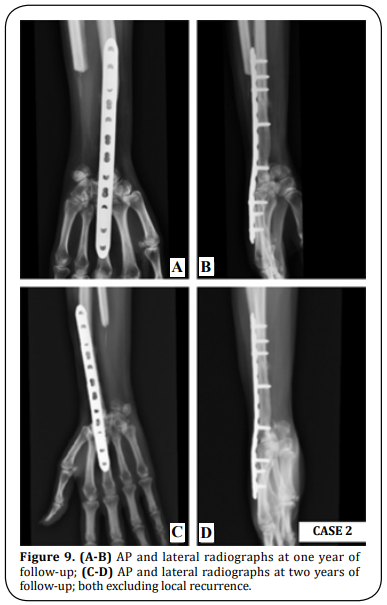
A 25-year-old right-hand dominant female presented with right wrist pain over an enlarging mass for one year. The patient reported a gradual increase in size over the last two months. On physical examination, the dorsal distal radius was tender and wrist motion was painful. The X-ray and CT scan revealed an expanded osteolytic lesion. MRI detected a huge osteolytic lesion and soft tissue extension with 4 x 3,3 x 2,3 cm, compatible with a Campanacci grade III GCTB (Figure 6). Staging imaging excluded other lesions. The histology report of the imaging-guided core biopsy showed a GCTB. After one year of denosumab therapy (120 mg SC per 28 days, during 12 months) (Figure 6) the patient underwent the same surgery as in Case 1. Wrist arthrodesis with a 3.5 mm LCP plate was performed after a 6 cm dorsal en-bloc resection of the distal radius and translocation of the ipsilateral ulna (Figure 7). There were no major complications related to the procedure. The histological report confirmed complete resection with free margins. An above-elbow cast was applied for three weeks, after which a belowelbow was used for two more weeks. After two months the patient had a full SN/PN and after six months the patient was able to perform the daily activities without restrictions or pain (Figure 8). At six months the MSTS score was 24 (compared to the pre-operative value of 19), the mean handgrip strength value for the operated side was 33,1 lbs compared to 49,8 lbs for the non-operated side, and scored 27,3 in Quick-DASH questionnaire (the same value as in the pre-operative assessment). At two years of follow-up, the patient has no clinical or imaging signs of local recurrence (Figure 9).
Discussion
GCTB of GCTB of the distal radius is the third most
common site of this relatively rare neoplasm,
corresponding to 10% of all cases [2, 4-7, 17, 18]. Despite
its benign label, the distal radius is the most common
primary site responsible for metastases and a
high focus on ruling out pulmonary metastasis is
mandatory in the pre-operative assessment [9, 10, 12, 19].
In well-marginated cortical borders,
curettage
with
bone grafting/cement packing is acceptable despite
the recurrence rates up to 50% [4, 5, 7, 17, 19]. Campanacci grade, pathological fractures, tumor
site, and
adjuvant
therapy are recognized predictors of local recurrence [1, 19]. Studies have correlated the incidence
of metastases
with aggressive growth and local recurrence [20, 21].
The treatment of the rare Campanacci III
lesions is
a much more arduous task. Wide resection must be
performed to avoid recurrence and reconstructive
options should be considered to preserve wrist
function. The en-bloc resection is widely acceptable
in expansive lesions, recurrent tumors, and when
the articular surface is largely damaged or collapsed
[17, 18, 22]. Due to the proximity with other bones (ulna
and carpal bones) and other soft tissue structures,
intralesional excisions, even when adjuvant therapies
are used, have poor local control when compared to enbloc
resection [1,2]. Reconstruction of the wrist by ulnar
translocation after total resection was first described
in 1982 by Seradge [5, 6, 19, 22] and several techniques to
fixate the transposed ulna were described: Steinmann
pins, T-shape plates, dynamic compression plates,
cloverleaf plates, and K-wires [19]. The ipsilateral ulnar
translocation technique is a surgical procedure that avoids donor site morbidity and allows an adequate
muscular cover with improved vascularity [5, 7, 9, 17]. Furthermore, the option of a single bone in
the
forearm avoids the complication of ulnar variance
when other reconstruction techniques - fibular, iliac
crest, allografts - are considered [6]. When compared
with the proximal vascularized fibula, the ipsilateral
autologous ulna does not require microsurgical skills
[7, 17]. Autologous ulna also eliminates the risk of graft
rejection [5]. Comparing all the fixation methods of the
translocated ulna, Chobpenthai et al. [19]. concluded that
distal radius plating is the less traumatic technique
and achieves the best functional and cosmetic results.
Despite the flaws pointed out to this technique
(poor
vascularity, proximal and distal nonunion, and lack
of motion), arthrodesis results in less post-operative
pain and good to excellent results in grip strength [15, 19]. The most accepted wrist position after
fusion is 10°
dorsiflexion and 5-10° ulnar deviation [9].
Another possibility for reconstruction could be a
custom-made mega prosthesis to preserve some
motion in the sagittal e coronal planes. However, the
literature is scarce and these patients were too young
and with some functional demand, so the arthroplasty
would be quickly condemned to fail [23].
No less important is the role of denosumab, used as
neoadjuvant therapy, in making tumor dissection
viable. The massive cortical destruction and friable
nature of GCTB benefit from this chemotherapeutic
agent in reducing pain and suppressing the tumor [1, 10].
In conclusion, although treatment of Campanacci
grade III GCTB of the distal radius remains a challenge,
the combination of neoadjuvant denosumab therapy
and tumor en-bloc resection have a good prognosis.
The reported reconstructive technique achieved good
functional and oncological outcomes.
Declarations
Acknowledgments
Work performed at Orthopaedics Department of Centro Hospitalar e Universitário do Porto, Porto, Portugal. The authors would like to thank Luís Oliveira for his help in the preparation of the manuscript.
Author's contributions
All the authors contributed substantially to the designand production of this article.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
This study, which included human samples was written informed consent was obtained from the patients for publication of these case reports and any accompanying images. All studies involving human subjects were in accordance with the Helsinki Declaration.
References
1. Zou, C., Lin, T., Wang, B., Zhao, Z., Li, B., Xie, X., ... &
Shen, J. (2019). Managements of giant cell tumor
within the distal radius: a retrospective study
of 58 cases from a single center. Journal of bone
oncology, 14, 100211.
2. Liu, Y.-p., Li, K.-h., & Sun, B.-h. (2012). Which
treatment is the best for giant cell tumors of
the distal radius? A meta-analysis. Clinical
Orthopaedics and Related Research, 470(10),
2886-2894.
3. Sánchez-Torres, L., de la Parra-Márquez, M., Cruz-
Escalante, A., Ramírez-Barroso, R., & Espinoza-
Velazco, A. (2017). Microsurgical reconstruction in
limb salvage due to a giant cell tumor of the distal
radius. Case report. Acta ortopédica mexicana,
31(2), 98-102.
4. Wang, Y., Min, L., Lu, M., Zhou, Y., Wang, J., Zhang,
Y., ... & Duan, H. (2020). The functional outcomes
and complications of different reconstruction
methods for Giant cell tumor of the distal radius:
comparison of Osteoarticular allograft and
three-dimensional-printed prosthesis. BMC
musculoskeletal disorders, 21(1), 1-15.
5. Salunke, A. A., Shah, J., Warikoo, V., Chakraborty,
A., Pokharkar, H., Chen, Y., ... & Pandit, J. (2017).
Giant cell tumor of distal radius treated with ulnar
translocation and wrist arthrodesis: What are
the functional outcomes? Journal of Orthopaedic
Surgery, 25(1), 1-6.
6. Puri, A., Gulia, A., Agarwal, M., & Reddy, K. (2010).
Ulnar translocation after excision of a Campanacci
grade-3 giant-cell tumour of the distal radius: an
effective method of reconstruction. The Journal of
bone and joint surgery British volume, 92(6), 875-
879.
7. Ververidis, A. N., Drosos, G. I., Tilkeridis, K. E., &
Kazakos, K. I. (2015). Carpus translocation into the
ipsilateral ulna for distal radius recurrence giant
cell tumour: a case report and literature review.
journal of orthopaedics, 12, S125-S129.
8. Xu, L., Jin, J., Hu, A., Xiong, J., Wang, D., Sun, Q., &
Wang, S. (2017). Soft tissue recurrence of giant cell
tumor of the bone: prevalence and radiographic
features. Journal of bone oncology, 9, 10-14.
9. Vyas, A., Patni, P., Saini, N., Sharma, R., Arora, V., &
Gupta, S. (2018). Retrospective analysis of giant
cell tumor lower end radius treated with En bloc
excision and translocation of ulna. Indian journal
of orthopaedics, 52(1), 10-14.
10. Van Handel, A. C., Galvez, M. G., Brogan, D. M.,
Boyer, M. I., Cipriano, C. A., Hirbe, A. C., & Pet, M.
A. (2020). Vascularized Ulnar Transposition and
Radioulnoscapholunate Fusion With Volar Locking
Plate in a Dorsal Position Following Resection of
Giant Cell Tumor of the Distal Radius. Techniques
in hand & upper extremity surgery, 24(3), 142-
150.
11. Lieberman, J. R. AAOS Comprehensive Orthopaedic
Review 3: Lippincott Williams & Wilkins; 2019.
12. Chalidis, B. E., & Dimitriou, C. G. (2008).
Modified ulnar translocation technique for the
reconstruction of giant cell tumor of the distal
radius. Orthopedics (Online), 31(6), 1.
13. Palacios, A. O., Ambite, J. C. M., & Zbigniew. (2018).
Giant Cell Tumors on the Fourth Metacarpal: about
a case. Revista Iberoamericana de Cirugía de la
Mano, 46, 40-45.
14. Cheng, C.-Y., Shih, H.-N., Hsu, K.-Y., & Hsu, R. W.-W.
(2001). Treatment of giant cell tumor of the distal
radius. Clinical Orthopaedics and Related Research
(1976-2007), 383, 221-228.
15. Zhang, J., Li, Y., Li, D., Xia, J., Li, S., Yu, S., ... &
Yang, Z. (2016). Clinical effects of three surgical
approaches for a giant cell tumor of the distal
radius and ulna. Molecular and clinical oncology,
5(5), 613-617.
16. Saikia, K. C., Bhattacharyya, T. D., Bhuyan, S.
K., Bordoloi, B., Durgia, B., & Ahmed, F. (2011).
Local recurrences after curettage and cementing
in long bone giant cell tumor. Indian journal of
orthopaedics, 45(2), 168-173.
17. Meena, D. K., Thalanki, S., & Sharma, S. B. (2016).
Wrist fusion through centralisation of the ulna for
recurrent giant cell tumour of the distal radius.
Journal of Orthopaedic Surgery, 24(1), 84-87.
18. Saini, R., Bali, K., Bachhal, V., Mootha, A. K., Dhillon,
M. S., & Gill, S. S. (2011). En bloc excision and
autogenous fibular reconstruction for aggressive
giant cell tumor of distal radius: a report of
12 cases and review of literature. Journal of
orthopaedic surgery and research, 6(1), 1-9.
19. Chobpenthai, T., Thanindratarn, P., Phorkhar, T., &
Ingviya, T. (2020). The reconstruction after en-bloc
resection of giant cell tumors at the distal radius:
A systematic review and meta-analysis of the ulnar
transposition reconstruction technique. Surgical
Oncology, 34, 147-153.
20. Bertoni, F., Present, D., Sudanese, A., Baldini, N.,
Bacchini, P., & Campanacci, M. (1988). Giant-cell
tumor of bone with pulmonary metastases. Six
case reports and a review of the literature. Clinical
orthopaedics and related research, (237), 275-
285.
21. Siebenrock, K., Unni, K., & Rock, M. (1998). Giantcell
tumour of bone metastasising to the lungs: a
long-term follow-up. The Journal of bone and joint
surgery British volume, 80(1), 43-47.
22. McLean, J. M., Clayer, M., Stevenson, A. W.,
& Samson, A. J. (2014). A modified ulnar
translocation reconstruction technique for
Campanacci grade 3 giant cell tumors of the distal
radius using a clover leaf plate. Techniques in hand
& upper extremity surgery, 18(3), 135-142.
23. Hariri, A., Facca, S., Di Marco, A., & Liverneaux,
P. (2013). Massive wrist prosthesis for giant cell
tumour of the distal radius: a case report with a
3-year follow-up. Orthopaedics & Traumatology:
Surgery & Research, 99(5), 635-638.