Open Access | Research Article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Clinical Application and Efficacy Analysis of 3D Navigation Module in the Treatment of Atlantoaxial Instability
*Corresponding author: Yong-xiong He, Department of Spine Surgery, Inner Mongolia People’s Hospital, Saihan District Zhao wuda road No.42, Hohhot 010017, Inner Mongolia, China.
E-mail: spinedoctor@sina.com
Received: 15 November 2018 Accepted: 15 December 2018 Published: 25 December 2018
DOI: 10.31491/CSRC.2018.12.023
Abstract
Background: Posterior cervical atlantoaxial pedicle screw fixation is a very effective treatment for atlantoaxial instability (AAI). However, due to the complex anatomy of the cranial-cervical junction, the accuracy and safety of posterior atlantoaxial pedicle screw placement remains extremely challenging.
Objective: To quantitatively evaluate the safety and accuracy of the 3D navigation module to assist the posterior atlantoaxial fixation.
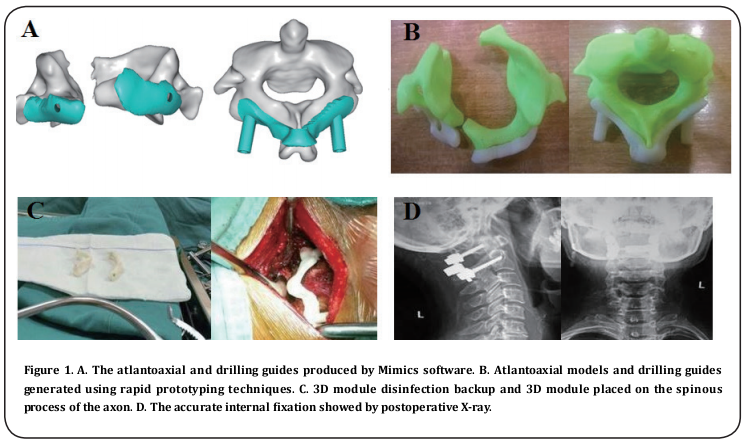
Methods: A total of 20 AAI patients were selected between June 2014 and September 2015. The Mimics v10.1 and 3-matic software were used. The 3D navigation module was designed as a double-sided positioning hole guide with a guide rod. All patients underwent posterior atlantoaxial posterior pedicle screw fixation with 3D navigation module. The actual entry point and screw trajectory were measured after operation, which were compared with the ideal entry point and screw trajectory. The Japanese Orthopaedic Association (JOA) score was measured before and after surgery to evaluate the neurological function improvement. The average operation time, blood loss, and frequency of intraoperative fluoroscopy were counted.
Results: The posterior atlantoaxial pedicle screw fixation with a 3D navigation module was successfully performed in all patients. A total of 80 atlantoaxial pedicle screws were implanted in the 20 patients. Postoperative CT scan showed that two pedicle screws deviated from the medial aspect of the atlas pedicle cortex and entered the spinal canal approximately 1 mm, without causing neurological complications. There was no significant difference between the ideal and actual entry points or ideal and actual screw trajectories of the atlas and axis (P > 0.05). The preoperative JOA score was 12.45 ± 1.15 and postoperative JOA score was 15.5 ± 0.89, with statistically significant difference (P < 0.05).
Conclusion: KIt was safe and effective to use the 3D navigation module to assist the posterior atlantoaxial pedicle insertion, with a high accuracy of pedicle screw placement.
Keywords
atlantoaxial instability; pedicle screw; 3D navigation module; rapid prototyping
Introduction
In recent years, patients with atlantoaxial instability (AAI) have been routinely treated with posterior atlantoaxial pedicle screw fixation [1-3]. The cervical spondylosis requiring internal fixation was generally caused by
multiple injuries and such injuries were often combined with fracture dislocation, leading to the destruction of its three-column structure. In 1994, Abumi, et al. [4] successfully applied and promoted the posterior cervical
pedicle screw fixation in the treatment of lower cervical injury. Because the pedicle screw fixed the three columns (anterior, median, and posterior) of the vertebral body and thus provided a good three-dimensional fixed pattern, it has
obvious advantages compared with other fixed methods by biomechanics [5]. However, as the cervical vertebra has a complex anatomical structure and an important adjacent relationship, and the pedicle is relatively slender with
great angle change, the most common and most serious surgical complications are C2 nerve root and vertebral artery injures that are caused by the pedicle screw trajectories deviating from the pedicle cortex [6], which makes
the clinical application of posterior cervical pedicle screw fixation extremely limited. Therefore, how to improve the accuracy of screw placement and reduce surgical complications is an important problem that needs to be solved urgently
in clinical work.
The cervical pedicle screw fixation methods currently used in the clinic include bare-handed screw-setting
[7], screw-setting assisted by the imaging techniques,computer-assisted orthopaedics surgery (CAOS) [8], and 3D printing technology that was also called computer- aided design-rapid prototyping (CAD-RP technology).
The key points of the bare-handed screw-setting are the accuracy of the point and direction of the screw, rich experience, and intraoperative fluoroscopy. The screw-setting assisted by the imaging techniques has high requirements for doctors'
knowledge accumulation, experience judgment, and spatial imagination, causing certain subjectivity and lacking objective measurement standards. CAOS makes intraoperative surgery more precise, safe and effective, but its expensive equipment
costs and operational complexity limit its promotion and application [9-11]. The CAD-RP technique was first applied to lumbar pedicle screw placement by Radermacher et al . [12]. It is a kind of modern digital orthopedic
technology. Its principle is to scan the structure of tissue and organ through CT, generate a proportional 3D module corresponding to the real object, and make a solid model proportional to the patient through the 3D printer; through the
solid model, the surgical simulation and intraoperative reference and application are performed
[10]. The rapid prototyping drill guide template designed by 3D printing technology can help improve the accuracy of the screw placement [13-16]. In this prospective clinical study, we designed a drill guide template
for atlantoaxial pedicle screw placement. The purpose of this study was to quantitatively evaluate the accuracy of placement of atlantoaxial pedicle screws using a drill guide template.
Materials and Methods
Subjects
All patients signed written informed consent. In addition, this study followed the principles outlined in the Helsinki Declaration. Patients with atlantoaxial instability (AAI) who were hospitalized and surgically treated in our hospital from June 2014 to September 2015 were enrolled in this prospective study. A total of 20 patients who underwent AAI posterior approach (17 Male and 3 female), with an average age of 42.6 years (age range 22-46 years), were selected based on the inclusion and exclusion criteria. All AAI patients underwent posterior atlantoaxial pedicle screw fixation with a drill guide template. All protocols have been approved by the Committee of Inner Mongolia People’s Hospital.
Diagnostic criteria: All patients were diagnosed with AAI by clinical and imaging examinations and had clinical symptoms.
Inclusion criteria: patients who meet the diagnostic criteria; patients who can be placed with the atlantoaxial pedicle screw by X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) examinations; patients whose surgeries were performed by the same senior physician.
Exclusion criteria: patients with severe vertebral injury, malformation, small posterior arch, etc.; patients with advanced age, combined with serious medical diseases and osteoporosis, unable to tolerate surgery; patients with infection, tuberculosis, tumor, and other complica-tions; patients who had a mental illness.
Construction of 3D navigation module
Software Platform
Mimics (Materialise's interactive medical image control system), known as "Dream Factory of Medical Imaging", is a medical image control system developed by Materialise of Belgium to realize interoperability. Through this software, various medical imaging materials such as CT, MRI, and other two-dimensional data are imported, and then the image data are analyzed by the clinician on three different orthogonal planes: cross-section, coronal plane, and sagittal plane. The valuable areas are optimized to get the desired data, and then the 3D data model is rebuilt. Through the surgical simulation operation, virtual surgical operations can be performed in the software, such as pre-surgical program and prosthesis placement. Mimics can perform 3D reconstruction of imaging data, providing support for a variety of supporting software applications such as virtual reality (VR), computer-aided design (CAD), finite element analysis (FEA), and rapid prototyping (RP). Therefore, Mimics can be used for clinical diagnosis, surgical simulation (pre-surgical program, virtual surgery operation, prediction and analysis of surgical risk), and can also be applied to anatomy teaching and scientific research. It has great potential for functional development [17].
3-matic is a forward engineering based on Digital Standard Triangle Language (STL) produced by Materialise. It can directly edit and modify STL format files to implement FEA/CFD processing in various STL formats. All operations of 3-matic are based on digital form (triangle based) for stretching, rotation, arraying, etc. It can directly copy and paste the anatomical data in Mimics software, and can input them into any CAD document. Through 3-matic, we can implement 3D measurement and engineering analysis, design implants and surgical guidelines for specific patient surgeries, and prepare anatomical data or implants for finite element simulations. This study used 3-matic to create a personalized navigation template for atlantoaxial pedicles, which greatly reduced the time required to create navigation templates using traditional reverse engineering [17].
Atlantoaxial pedicle screw simulation placement
All patients underwent cervical CT with a tomographic thickness of 0.625 mm. CT images were imported into Mimics software and the atlantoscopic 3D model was constructed. In the virtual environment of the Mimics software, a cylinder (3.5 mm in diameter) was created as an atlantoaxial pedicle screw, which is because it is easier to make and adjust the position of the cylinder in the software. The ideal trajectory of the atlantoaxial pedicle screw was created and adjusted by directly observing the relationship between the cylinder and the pedicle cortical bone in different planes.
Production of atlantoaxial 3D guide module
Then the 3D model of the atlantoaxial vertebral body and the cylinder was introduced into the 3-matic (Materialise) software to design a 3D drilling guide module with drilling guidance. In the 3-matic software, the surface of the template (2.5-mm thickness) was created as the opposite side of the posterior atlantoaxial surface, thus providing a perfect fit between the template and the posterior atlantoaxial surface. Using a Boolean subtraction operation, two position holes (3.5-mm diameter) were created on both sides of the template surface based on the data of the cylinder. After the cylinder was interactively translated, two guide holes (3.5-mm diameter) were created on the optimum entry points on either side of the template surface. The direction of the drill guide hole was exactly the same as the optimum nailing direction. The local Boolean operation was used to combine the drill guide hole and the template surface with the positioning hole into one unit .
Physical molding of 3D guides
The DICOM format of the cervical CT of the patient was introduced into the Mimics software, and the atlas template of interest was obtained by operation of thresholding, region growing, crop mask, editing mask, etc. Then the atlas template selected, followed by the click of the "Calculate 3D" button to complete the 3D reconstruction of the atlas. The 3D model of the atlas was displayed in the 3D viewport and was smoothed, reduced by triangle reduction, etc. The final 3D model of the atlas was obtained, and then imported into a 3D printer to print out the patient’s atlantoaxial model using a photosensitive resin material.
Surgical procedures
All operations were performed by the same senior surgeon. The patient was placed in the prone position under general anesthesia and the head was fixed by the Mayfield head frame. The median incision of the posterior neck was taken and separated layer by layer to fully reveal the posterior structure of the atlantoaxial vertebrae, including the posterior tibial tuberosity and posterior arch, lamina, and lateral vertebral blocks. The soft tissue covering the bony structure was completely peeled off by subperiosteal peeling to make the drill guide template to be fully compatible with the posterior surface of the vertebra. The drill guide was fixed and the guide hole was drilled through the template positioning hole, followed by the drilling of the trajectory parallel to the guide rod of the template. The probe was used to detect the four walls of the nailing channel were leaking. The intraoperative fluoroscopy was used to confirm that the drilled trajectory was ideal. If the actual trajectory deviated from the ideal trajectory due to the poor fit between the template and the posterior atlantoaxial surface, the direction of the drill was adjusted according to the template. After achieving the ideal spiral path, a 3.5-mm screw was inserted. The pre-bent rods were then secured to the sides of the atlantoaxial pedicle screws (Fig. 1). Decompression of the occipital foramen was then performed if necessary.
Postoperative treatment
The patient’s vital signs were closely observed. Postoperative routine hormones were given to prevent spinal cord inflammation and edema; antibiotics were given to prevent infection; meeobalamin was used for nourishing nerves. The drainage tube was routinely removed within 48 hours. The patient was routinely bedridden 3-5 d, with the axis turned over; after 3-5d, patients would go to the ground. The neck brace was worn for 3 months after operation, followed by the X-ray examination of the cervical spine. According to the results of the review, the neck brace was removed.
Evaluation of outcomes
Evaluation of screw trajectories
The accuracy of the atlantoaxial pedicle screw was analyzed by a physician who did not participate in surgical stapling. All patients had cervical CT scans after surgery. Preoperative and postoperative CT images were imported into Mimics software. The preoperative atlantoaxial 3D model and cylinder as well as the postoperative atlantoaxial 3D model and screw were reconstructed. The "global registration" operation was used to superimpose the preoperative 3D model with cylinder and the postoperative 3D model with the screw. This overlay facilitated the comparison of the cross-sectional angle and sagittal angle between the ideal screw trajectory with the actual screw trajectory. Besides, the patient was routinely examined by CT after surgery, and the picture archiving and communication system (PACS) measurement tool was used to display the relative positional relationship between the screw and the pedicle according to the CT slice. Screw-setting accuracy was evaluated by the methods provided by Yoshiharu et al. [18], Miyamoto et al. [19], and Yasutsugu et al. [20]. Grade 0: The screw is completely placed inside the pedicle; Grade I: the screw penetrates the pedicle bone cortex ≤ 2 mm, without neurological or vertebral artery injury and other complications associated with screw placement; Grade II: screw penetrates the pedicle bone cortex > 2mm, without neurological or vertebral artery injury and other complications related to nailing; Grade III: neurological or vertebral artery injury and other complications related to screw placement occur.
Evaluation of the entry points
In order to properly compare the ideal and actual coordinates of the entry point, the axis of the atlantoaxial axis was adjusted. For C1, the front nodule was treated as the origin of the coordinate axis. The x-axis passed through the origin of the coronal plane and was parallel to the line connecting the lowest points of the lower articular processes on both sides. The y-axis and the z-axis passed through the origin and were perpendicular to the x-axis of the horizontal and coronal planes, respectively. In the case of the C2 vertebra, the midpoint of the line connecting the lowest points of the articular processes on both sides was regarded as the origin. The y-axis and the z-axis passed through the origin and were perpendicular to the x-axis of the horizontal and coronal planes, respectively.
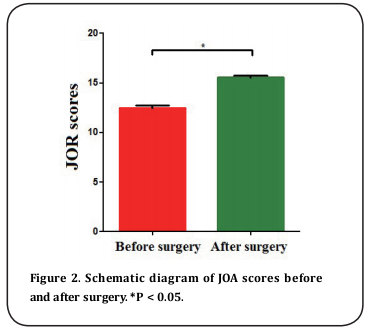
Evaluation of neurological function improvement
The JOA score was used to evaluate the neurological function of the patient before and 6 months after surgery. The score was divided into 17 points. The higher the score, the better the neurological function.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 statistical software. Data were expressed as mean ± standard deviation. The comparisons were performed using paired-sample t-test. P < 0.05 was considered as significantly different.
Results
Statistics of postoperative general results
All patients successfully underwent surgery with the aid of a drill guide template. Five of the 80 screws were placed in a direction that was adjusted during surgery, and a satisfactory screw trajectory was achieved after adjustment. No complications such as vertebral artery injury, cerebrospinal fluid leakage or spinal cord injury were found. Three patients developed venous plexus hemorrhage. The mean operative time was 174.3 ± 27.6 minutes and the mean bleeding volume was 312.9 ± 13.5 ml. The mean frequency of intraoperative fluoroscopy was 2.60 ± 0.68.
Comparison of JOA scores before and after surgery
The scores of the Japanese Orthopaedic Association (JOA) were compared between pre-surgery and 6 months after surgery. The preoperative JOA score was 12.45 ± 1.15 and postoperative JOA score was 15.5 ± 0.89, with statistically significant difference (P < 0.05) (Fig. 2).
Comparisons between the ideal and actual screw trajectories, entry points
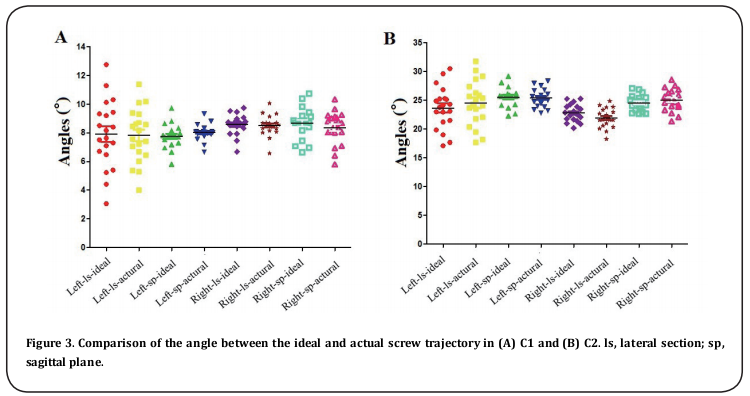
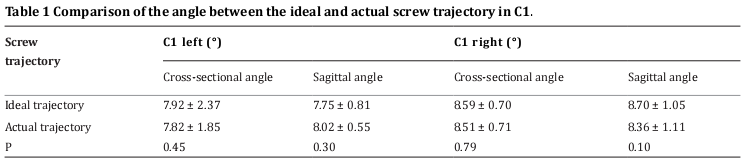
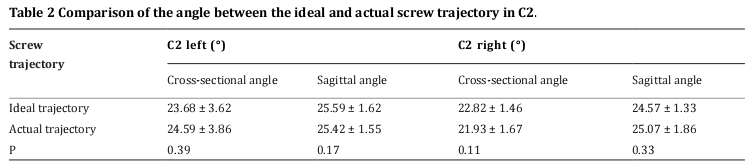
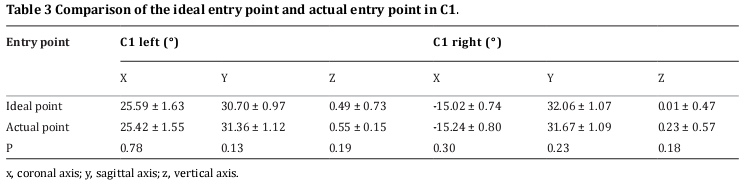
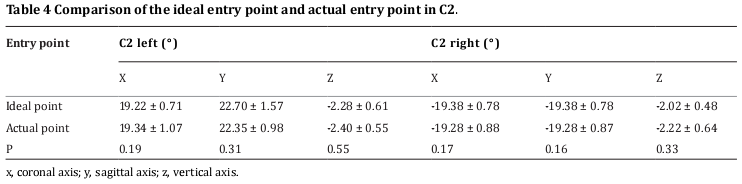
A total of 80 atlantoaxial pedicle screws were placed in 20 AAI patients. Postoperative CT scan showed 79 grade 0 screws and 1 grade I screw. One of the pivotal screws deviated inwardly from the pedicle cortex and entered the spinal canal approximately 1 mm, but no neurological and surgical complications occurred. There was no significant difference in the mean cross-sectional angle between the left (P = 0.45), right (P = 0.79) ideal screw trajectory and actual screw trajectory of atlas. No significant difference in the mean sagittal angle was observed between the left (P = 0.30), right (P = 0.10) ideal screw trajectory and the actual screw trajectory of atlas (Table 1 and Fig. 3A). Besides, there was no significant difference in the mean cross-sectional angle between the left (P = 0.39), right (P = 0.11) ideal screw trajectory and actual screw trajectory of axis. No significant difference in the mean sagittal angle was observed between the left (P = 0.17), right (P = 0.33) ideal screw trajectory and the actual screw trajectory of axis (Table 2 and Fig. 3B). As for the screw entry point coordinates, there was no significant difference between the ideal entry point and the actual entry point on both sides of the atlases, axises (P > 0.05) (Table 3 and Table 4).
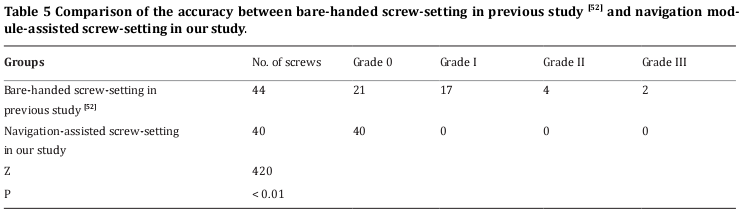
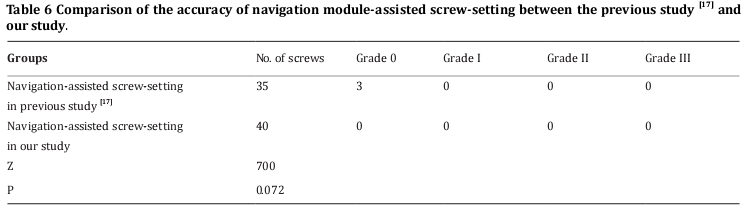
Comparison between bare-handed or navigation module-assisted screw-setting in previous study [17] and navigation module-assisted screw-setting in our study
In our study, using navigation module-assisted screw-setting, 40 screws were placed in the atlas with 40 screws of grade 0 (100%) and 40 screws were placed in the axis with 39 screws of grade 0 (97.5%) and 1 screw of grade I (2.5%).
In the reference [17], using bare-handed screw-setting, 44 screws were placed in the atlas, with 21 screws of grade 0 (47.7%), 17 screws of grade I (38.6%), 4 screws of grade II (9.14%), and 2 screws of grade III (4.5%); using navigation module-assisted screw-setting, a total of 38 screws were placed with 35 screws of grade 0 (92. 1%) and 3 screws of grade I (7.9%).
In our study, grade 0 and grade I screws were considered as satisfactory screws. The satisfaction rate of atlantoaxial screw placement in this study was 100% (40/40; 40/40). In the reference [17], the satisfaction rate was 86.3% (38/44) for bare-handed screw-setting and was 100% (38/38) for navigation module-assisted screw-setting.
Using the rank sum test analysis, the accuracy of screw-setting was significantly improved in our study compared with the bare-handed screw-setting group of the reference (P < 0.01). Further, there was no significant difference in the accuracy of navigation module-assisted screw-setting between our study and the reference (P > 0.05)(Tables 5 and 6).
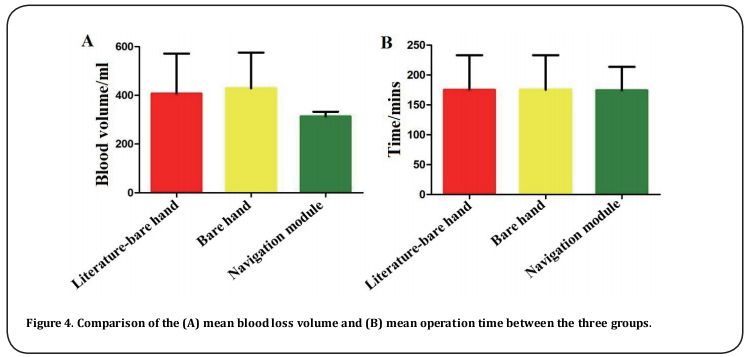
Comparison of postoperative general results between the previous study [17] and our study
The average operation time of our study was 174.3 ± 27.6 min, with the average blood loss of 312.9 ± 13.5ml. Referring to the previous literature [17], for bare-handed screw-setting and navigation module-assisted screw-setting, the average operation time was 175 ± 41 min and 175 ± 41 min with the average blood loss of 407 ± 116 ml and 428 ± 104 ml, respectively. Since there was no detailed data in the reference, simple comparisons can only be made with mean ± standard deviation. The average operation time of this study was similar to that of the reference, but the average amount of bleeding was slightly reduced (Fig. 4A and B). Finally, typical cases and special cases were shown in supplementary Fig. 1-3.
Discussion
Cervical pedicle screw placement is a difficult point in spinal surgery. This is related to the particularity of the atlantoaxial anatomy, which also leads to the risk of surgery under normal anatomy, and surgery is more challenging when fractures and dislocations occur in this area [21]. Therefore, clinically, atlantoaxial fixation is difficult and has a high potential risk, and it has been called a surgical "forbidden zone". CAD-RP technology can accurately control the patient's anatomy and individual differences before surgery, thus improving the accuracy of atlantoaxial screw-setting. Jiang et al . [22] used 3D navigation modules to assist the placement of 128 atlantoaxial pedicle screws in 32 patients with AAI. Postoperative CT showed that the atlas had two screws protruding into the spinal canal < 1mm without causing related complications. Although the anatomical structure of the lower cervical vertebra is not more specific than the atlantoaxial vertebrae, it is one of the difficult factors for screw placement due to individual differences and damage [23-25]. In addition, Kaneyamade et al . [26] applied a 3D navigation module to assist the placement of 80 screws in the lower cervical spines of 20 patients; after surgery, all 80 screws were found in the pedicle without related complications.
In the present study, the guide template of this study also selects the type of single-vertebral double-sided drilling guide plate which is currently used more. This type of drilling guide plate can select the spinous process as a fixed site and has double-sided drilling guide plate, which can be well fixed during operation. The drill guide has the advantage of drilling direction, and intuitively presents the direction of the screw. If necessary, it can help to adjust the direction of the screw. We found that a screw of the vertebral pedicle deviated inwardly from the pedicle cortex and entered the spinal canal approximately 1 mm, but there was no symptom. This deviation may be caused by the failure to remove the soft tissue during surgery, possibly resulting in insufficient fit between the template and the posterior vertebral surface. Therefore, the soft tissue on the posterior arch surface of the atlas should be completely removed before applying the drill guide template. In previous studies, the efficacy of spinal screw placement was demonstrated in a bilateral guide template. In the cadaveric study, Hu et al. [27] placed 64 C1 pedicle screws and 64 C2 pedicle screws without causing a screw to penetrate the cortex. However, it should be noted that the subject is a cadaver. The factors that may affect the results are listed as follows: preoperative and postoperative CT scans can be consistent in position; during the operation, the exposure and peeling of the operation area can be revealed and peeled off as much as possible.
Regarding the assessment of screw placement accuracy, some studies have simply reported the extent of screw insertion into the spinal canal in postoperative CT scans [28]. In this study, we also made more accurate evaluation criteria in addition to the statistics of the degree of screw insertion into the spinal canal. After using the 3D navigation module to assist the placement of the screw, the CT scan was first performed on the postoperative patients. The high-quality rate of the screw-setting was evaluated by the method developed by Yoshiharu et al. [18]. A total of 80 individual screws were placed in the personalized navigation template group, of which 79 were grade 0 and 1 was grade I, with the screw-setting satisfaction rate was 100%. Although this CT scan-based method helps to make the overall evaluation of the screw position, it cannot help to effectively compare the ideal and actual trajectories of the screw. Hu et al . [27] analyzed the positional deviation of C2 laminar screws from the ideal and actual entry points as well as trajectory directions. Hu et al. superimposed the preoperative and postoperative atlantoaxial models in Mimics software and compared the ideal and actual screw trajectories. This is a more efficient way to compare the ideal and actual screw trajectories. In this study we also used this method to compare the ideal and actual screw trajectories. The results showed that the application of the drill guide module to assist the placement of the pedicle screw was extremely accurate, and there was no statistical difference between the two screw trajectories. The evaluation of the two screw trajectories can not only overall reflects the satisfaction rate of screw-setting, but also analyzes the ideal and actual screw trajectory angles in different planes, making the evaluation of screw-setting accuracy more perfect.
The average operation time in this study was similar to that in the previous study [17]. However, the average blood loss of this study was significantly lower than that in the reference [17], possibly due to the following points. First, there were differences in the number of experimental subjects: 20 subjects in this study, 22 cases in the bare-handed screw-setting group of the reference, and 19 cases in the navigation moduleassisted screw-setting group of the reference. Second, the differences in the intraoperative situation and the patient's own situation. The age of patients in our study was significantly different from the overall age of the reference. The maximum age of the experiment was 46 years, and the maximum age of the reference was 64 years. Finally, intraoperative application of devices and personal operating habits may also be the cause. Besides, we found that the amount of bleeding in the navigation module-assisted screw-setting group was higher than that in the bare-handed screw-setting group [17], possibly resulting from the pursuit of the fitting degree of the guide to increase the extent of the vision field and soft tissue peeling during the use of guide templates. We believe that when using 3D navigation templates, we should combine the actual situation in the operation, and reduce the degree of peeling as much as possible without affecting the accuracy of screw placement.
During the operation of this study, it was found that the texture of the material used in the navigation template, a photosensitive resin material, was relatively soft and slight deformation occurred during use, which may be one of the causes of errors in this experiment. Owing to the diversity of materials of 3D printing technology, metal materials would be used to make navigation templates in the subsequent surgeries, which may eliminate related problems in this study. Besides, considering that the operating rooms of most lower-level hospitals may not be equipped with plasma disinfection equipment, the upgraded materials can also be used in the operating room without plasma disinfection equipment, which is conducive to clinical promotion. Further, in the early stage of the surgery, the surgeon with relatively lack of experience was selected for operation, resulting in a decrease in the satisfaction rate of the screw-setting. The postoperative X-ray film clearly showed the screw offset, but no neurological complications. Therefore, we believe that 3D navigation template-assisted screw-setting can greatly improve the accuracy of screw placement, but it is not omnipotent. This method still requires the operation of a physician with certain experience, and there is also a certain requirement for the understanding and proficiency of the use of the guide in case of emergency. However, the guide template is still positive for the guidance of young physicians, which can greatly reduce the learning curve and improve the accuracy of screw placement.
After this stage of surgery accumulation, we have two thoughts on the 3D navigation module. First of all, most of the currently used navigation module materials are photosensitive resin materials. In this study, the problems caused by the disinfection and use of materials have highlighted the limitation of the 3D navigation module itself. We consider further optimized materials as metal 3D navigation modules. Secondly, we encountered a deviation in the use of navigation templates due to poor chimerism, affecting the accuracy and safety of the screw placement. We believe that if the guide rod of the external screw-setting angle can be added during the production of the navigation template, the accuracy and safety of the screw-setting may be further improved. When a similar problem is encountered, even if the navigation template is not well fitted, the guide rod can still guide the screw placement.
In conclusion, the use of 3D navigation module is safe and effective for atlantoaxial pedicle screw implantation, which can significantly improve the accuracy of screw placement and prevent surgical complications. Therefore, the 3D navigation module-assisted posterior atlantoaxial fixation is worthy of clinical application.
References
1. Mingsheng, T., Huimin, W., Yunting, W., Guangbo, Z., Ping, Y., Zirong, L., Hongyu, W., and Feng, Y. (2003) Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine 28, 888-895
2. Lee, M. J., Cassinelli, E., and Riew, K. D. (2006) The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine (Phila Pa 1976) 31, 2798-2801
3. Jin, S. Y., Kafle, D., Nguyen, N. Q., Noh, W., Park, K. W., Chang, B. S., Lee, C. K., and Riew, K. D. (2012) Routine insertion of the lateral mass screw via the posterior arch for C1 fixation: feasibility and related complications. Spine Journal 12, 476-483
4. Abumi, K., ., Itoh, H., ., Taneichi, H., ., and Kaneda, K., . (1994) Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 7, 19-28
5. Ito, Z., Higashino, K., Kato, S., Kim, S. S., Wong, E., Yoshioka, K., and Hutton, W. C. (2014) Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: a biomechanical study on strength of fixation. Clinical Spine Surgery 27, 80-85
6. Gebauer, M., Barvencik, F., Briem, D., Kolb, J. P., Seitz, S., Rueger, J. M., Püschel, K., and Amling, M. (2010) Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. European Spine Journal 19, 85-90
7. Xu, R. (2009) A free-hand technique for pedicle screw placement in the lower cervical spine. Orthopaedic Surgery 5, S113-S114
8. Nolte, L. P., and Beutler, T. (2004) Basic principles of CAOS. Injury-international Journal of the Care of the Injured 35, 6-16
9. Steinmann, J. C., Mirkovic, S., ., Abitbol, J. J., Massie, J., ., Subbaiah, P., ., and Garfin, S. R. (1990) Radiographic assessment of sacral screw placement. Journal of Spinal Disorders 3, 232-237
10. Wang, M., and Wand, J. (2005) Application of computer aided navigation orthopedic surgery and medical robot technology in orthopedic trauma. Chinese journal of orthopedics and traumatology 7, 8-13
11. Laine, T., Lund, T., Ylikoski, M., Lohikoski, J., and Schlenzka, D. (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. European Spine Journal 9, 235-240
12. Radermacher, K., Portheine, F., Anton, M., Zimolong, A., Kaspers, G., Rau, G., and Staudte, H. W. (1998) Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop 354, 28 -38
13. Lu, S., Zhang, Y. Z., Wang, Z., Shi, J. H., Chen, Y. B., Xu, X. M., and Xu, Y. Q. (2012) Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Medical & Biological Engineering & Computing 50, 751-758
14. Taku, S., Naoki, H., Shuichi, K., Masato, T., Naoko, W., Fujio, U., Masatoshi, S., and Kazuo, M. (2013) Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine: clinical article. Journal of Neurosurgery.Spine 19, 185-190
15. Shuichi, K., Taku, S., Masatoshi, S., Naoki, H., Masato, T., and Kazuo, M. (2014) A novel screw guiding method with a screw guide template system for posterior C-2 fixation: clinical article. Journal of Neurosurgery Spine 21, 231- 238
16. Putzier, M., Strube, P., Cecchinato, R., Lamartina, C., and Hoff, E. (2017) A New Navigational Tool for Pedicle Screw Placement in Patients with Severe Scoliosis: A Pilot Study to Prove Feasibility, Accuracy, and Identify Operative Challenges. Clin Spine Surg. 30, E430-E439
17. Dong, C. (2016) Clinical study of comparison between personalized navigation template assisted atlas pedicle screw placement and freehand screw placement, Beijing University of Chinese Medicine 50, 751-758
18. Yoshiharu, K., Masato, N., Taketoshi, Y., Shoji, S., Takeshi, H., and Tomoatsu, K. (2012) Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide. Spine 37, 1983-1988
19. Miyamoto, H., and Uno, K. (2009) Cervical pedicle screw insertion using a computed tomography cutout technique. Journal of Neurosurgery Spine 11, 681-687
20. Yasutsugu, Y., Fumihiko, K., Keigo, I., Yumiko, H., Tetsurou, H., Hiroaki, N., and Masaaki, M. (2009) Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. European Spine Journal 18, 1293-1299
21. Duhem, R., Tonnelle, V., Vinchon, M., Assaker, R., and Dhellemmes, P. (2008) Unstable upper pediatric cervical spine injuries: report of 28 cases and review of the literature. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 24,343-348
22. Jiang, L., Dong, L., Tan, M., Yang, F., Yi, P., and Tang, X. (2016) Accuracy assessment of atlantoaxial pedicle screws assisted by a novel drill guide template. Archives of orthopaedic and trauma surgery 136, 1483-1490
23. He, Y., Liu, B., Zhang, L., Wang, D., Bao, C., Dong, J., Liu, C., Yu, H., Liu, B., and Peng, Y. (2013) Individualized treatment of atlantoaxial vertebra and matters needing attention. Chinese journal of clinicians (electronic edition), 193-194
24. Yang, S. Y., Boniello, A. J., Poorman, C. E., Chang, A. L., Wang, S., and Passias, P. G. (2014) A review of the diagnosis and treatment of atlantoaxial dislocations. Global spine journal 4, 197-210
25. Huang, X., Li, F., Zhang, F., Wang, K., Wang, Z., Yang, Q., Dang, R., Su, J., Shen, H., and Li, M. (2014) Experimental study of cervical pedicle screw placement assisted by individualized 3d printing navigation template. Chinese journal of orthopaedic surgery 22, 1880-1884
26. Kaneyama, S., Sugawara, T., and Sumi, M. (2015) Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine (Phila Pa 1976) 40, E341-348
27. Yong, H., Zhen-Shan, Y., Kepler, C. K., Albert, T. J., Hui, X., Jian-Bing, Y., Wei-Xin, D., and Cheng-Tao, W. (2014) Deviation analysis of atlantoaxial pedicle screws assisted by a drill template. Orthopedics 37, 420-427
28. Ma, T., Xu, Y. Q., Cheng, Y. B., Jiang, M. Y., Xu, X. M., Xie, L., and Lu, S. (2012) A novel computer-assisted drill guide template for thoracic pedicle screw placement: a cadaveric study. Archives of Orthopaedic & Trauma Surgery 132, 65-72Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 49, i6-16