Open Access | Mini Review
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Research advances in stem cell transplantation combined with fibrin scaffold for spinal cord injury in an aging society
# Tianqi Jiang and Zhijun Chen contributed equally to this work.
* Corresponding author: Yongxiong He
Mailing address: Department of Spine Surgery, Second Affiliated Hospital of Hainan Medical University, Haikou 570100, Hainan, China.
Email: spinedoctor@sina.com
* Corresponding author: Hua Yang
Mailing address: Baotou Central Blood Station, Baotou 014030, Inner Mongolia Autonomous Region, China
Email: lgf-ylf@163.com
DOI: 10.31491/APT.2024.03.137
Abstract
Older patients with spinal cord injury (SCI) had higher injury severity scores, longer hospital stays, and were significantly more likely to be discharged to an institution rather than younger patients. Treating SCI and promoting neural tissue regeneration is a major challenge for current medical technologies in an aging society. Tissue engineering scaffolds can provide a microenvironment suitable for cell survival and promote nerve tissue regeneration, and thus have become a promising therapeutic intervention. Among them, fibrin scaffold has become one of the most promising scaffolds for spinal cord regeneration due to its excellent biocompatibility, biodegradability, and high degree of integration with tissues. This article reviews the characteristics of an ideal fibrin scaffold and the role of fibrin scaffolds in the treatment of SCI in aging patients. Meanwhile, we explore the potential of stem cell transplantation combined with fibrin scaffold for the treatment of SCI. Through extensive and in-depth studies, this review will serve as a practical guide for the development of applications of fibrin scaffold combined with stem cell transplantation and provide direction for possible future work.
Keywords
Fibrin scaffolds, stem cells, spinal cord injury, tissue engineering scaffolds, aging
Introduction
Spinal cord injuries (SCI) are often caused by motor vehicle collisions. The occurrence of SCI not only causes severe physical
and psychological damage to the patients themselves but also imposes an enormous economic burden on families and society
[1]. When the spinal cord is damaged, the connection between the brain and the body is
forcibly interrupted, resulting in severe sensory and motor dysfunction of the limbs below the damaged segment. The characteristics
of SCI patients have changed as the population has aged. In a previous report from the United States, older patients in the acute
phase had higher injury severity scores, longer hospital stays, lower Glasgow Coma Scale scores, and were significantly more likely
to be discharged to an institution rather than younger patients [2]. According to the new
standard of 7% of the total population aged 65 years, 91 countries in the world have now entered into an aging society, including
Japan, Italy, and Germany. Therefore, how to treat late-life SCI in an aging society becomes a very delicate issue.
The pathophysiological mechanisms after SCI include primary and secondary injury. The initial mechanical trauma causes a primary
injury, such as tissue hemorrhagic edema and neuronal cell necrosis in the injured spinal cord, which subsequently triggers severe
secondary injury, such as tissue ischemia and necrosis, nerve conduction fiber fragmentation, demyelination, and glial scar
proliferation. This cascade of pathological changes leads to endogenous spontaneous repair processes that contribute little to the
recovery of spinal cord function [3, 4]. In
addition, a large amount of tissue loss occurs after severe SCI, resulting in a glial/fibrotic scar at the center of the SCI site
that continues to expand over time, leading to further tissue injury [5].
Currently, there are medical symptomatic, physiotherapeutic rehabilitation, stem cell transplantation, and surgical intervention
modalities used to treat SCI in aging people, but there is no single treatment modality that can completely restore the injured
spinal cord structure and function. The reasons for the failure of spinal cord regeneration are mainly attributed to the following
two points: poor axonal regeneration ability and the inhibitory hostile microenvironment at the injured site after trauma
[6]. When the central nervous system is injured, a large number of glial cells,
macrophages, and stromal cells are accumulated at the injury site. Subsequently, molecules that inhibit the axon growth, such as
chondroitin sulfate proteoglycan, are accumulated, eventually leading to the formation of glial scar, the lack of neurotrophic
factors, the destruction of myelin, and the demyelination of axons and other secondary injuries. This series of secondary injuries
impeded the growth of axons toward synapses, forming a physical and chemical barrier to spinal cord regeneration, ultimately
leading to the failure of spinal cord regeneration
[7-9] (Figure 1A).
Currently, the research hotspot for SCI in the elderly focuses on the mechanistic aspects of spinal cord regeneration, including
biological stem cell transplantation, tissue engineering, gene therapy, and drug screening, among which stem cell transplantation
is one of the high-potential approaches [10].
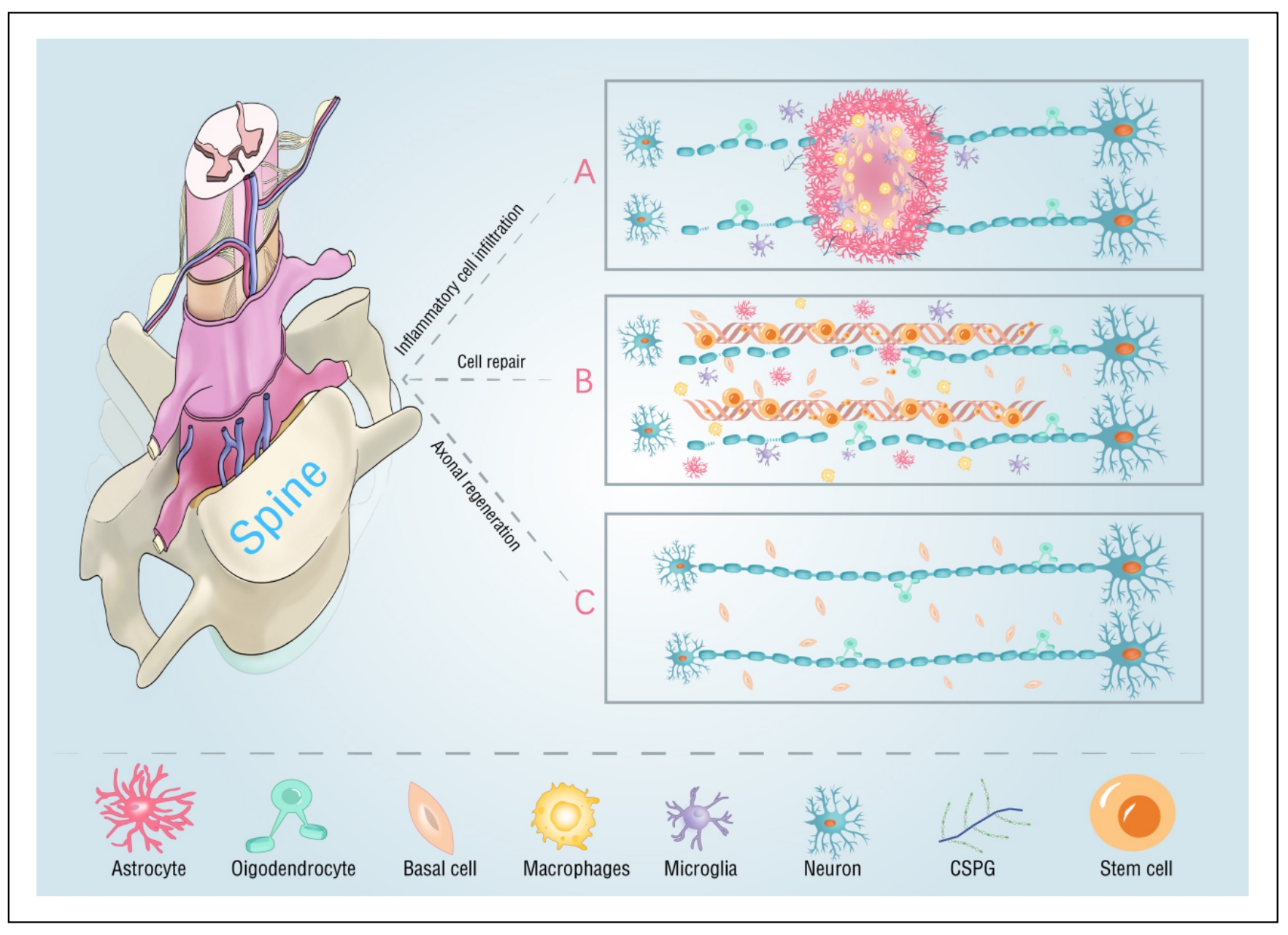
Figure 1. (A) After SCI, inflammatory cells infiltrated and wrapped around the damaged axons, forming a glial scar that impedes axon regeneration. (B) Some repair mechanisms after transplantation of fibrin scaffold containing stem cells into the injured spinal cord. The number of neurons and oligodendrocytes differentiated from the transplanted cells increased, and the number of other inflammatory cells decreased. (C) The axon regeneration and neural circuit recovery after transplantation of fibrin scaffold and stem cells.
Stem cells, which are used for transplantation, have the function of self-renewal. They can differentiate into glial cells or
neural progenitor cells (NPCs) along specific neural lineage under the appropriate environment, so as to replace and renew the
necrotic or apoptotic cells in the injured area, ultimately repairing the damaged spinal cord [11].
Research has discovered that aging-related secretory phenotype manifests in the spinal cord of aged mice following injury,
enhancing the suitability of the injury microenvironment for cell transplantation in aged mice
[12-14]. This suggests that the aged spinal
cord may provide a favorable environment for stem cell transplantation in older individuals. However, the analysis of SCI in
elderly rats has led to the conclusion that age is a factor influencing functional recovery, as it is associated with increased
axonal injury and demyelination [15]. This is consistent with the observed higher
activation of microglial cells, oxidative stress, and expression of inflammation-related genes in elderly rats following SCI
compared to young rats [16-18]. This increases
the likelihood of axonal growth impairment occurring after stem cell transplantation into the injured area. Studies have found
that tissue engineering scaffold technology can provide support and guidance for newly generated axons while preventing newly
generated axons from being damaged by scar tissue, thereby improving the survival rate of transplanted cells
[19].
Tissue engineering scaffolds can provide a suitable microenvironment for cell survival, limit local inflammatory responses, inhibit
apoptosis, promote nerve regeneration, and promote axon myelination [20]. Among them,
the fibrin scaffold has emerged one of the most promising scaffolds for spinal cord regeneration in the elderly, owing to its
excellent biocompatibility, biodegradability, and tissue integration capabilities [21].
Fibrin is a blood clotting protein synthesized by the liver. It is one of the most important proteins for promoting blood
coagulation, accelerating wound healing, and promoting tissue regeneration [22]. Fibrin
is formed by thrombin cleavage of fibrinogen in vivo and can spontaneously condense into three-dimensional multimers with
sponge-like structures. Based on this property, fibrin can be injected into the human injury site in liquid form and transformed
into a solid-state scaffold after entering the body [23], which may be useful for
improving the microenvironment of the injury site, aiding in cell transplantation as well as neuroprotection
[24, 25]. The results of a previous study
showed that neural stem cells (NSCs) expressing green fluorescent protein, when embedded in a growth factorrich fibrin matrix,
were transplanted into the injured spinal cord. The results showed that the transplanted stem cells differentiated into neurons and
helped the elongation of axons connect with the host cells to form rich synapses, which ultimately promoted the recovery of spinal
cord function [26].
In this review, we focused on the advantages and roles of fibrin scaffolds in promoting neurological functional recovery in the
elderly. Meanwhile, we summarized the potential that different types of stem cells combined with fibrin scaffolds in the treatment
of SCI, especially in the elderly. Finally, the challenges and prospects of stem cell transplantation combined with fibrin scaffold
application in SCI were pointed out.
Connections of fibrin scaffolds to SCI
As a fibrous biopolymer, fibrin can stop bleeding and promote wound healing by forming a temporary matrix around the lesion [27]. Fibrin is a component of the extracellular matrix, which aids in the repair of damaged areas by facilitating cell adhesion, binding to extracellular matrix proteins, and interacting with various growth factors [28]. The variation in the ratio of fibrinogen to thrombin can regulate the mechanical properties of fibrin hydrogels, thereby effectively treating spinal cord injuries in the elderly [29]. Clinical studies have found that local injection of a single dose of VX-210 or a placebo containing a fibrin sealant onto the injured dura mater during decompression/stabilization surgery may improve the quality of life in elderly patients with spinal cord injury [30]. Because of its high biocompatibility, fibrin can serve as a carrier for stem cell transplantation or as an injectable biomaterial to promote nerve regeneration. After SCI, while axons in the central nervous system cannot regenerate, they can promote axon healing by expanding new axon buds in the peripheral nerves [31]. According to this property, Tsai et al. [32] used fibrin matrix as a hollow nerve conduit to bridge the nerve defect area and encourage axon regeneration and growth. King et al. [25] injected fibrin/fibronectin into the injured part of the spinal cord in young adult male rats and observed new axon growth in the scaffold one week later. In addition, Lu et al. [26] found that the fibrin scaffold containing growth factors can effectively support the long-distance axon growth and interconnection of NSCs implanted with severe SCI in rats. It can be seen that fibrin, as a new natural scaffold material, holds promising research prospects for the repair of SCI.
Biological characteristics of suitable fibrin scaffolds
Scaffold materials are the foundation of tissue engineering scaffolds, and an ideal fibrin scaffold should possess the following properties.
Biocompatibility
Fibrin scaffolds play a role in directly contact with peripheral nerves and tissues. Therefore, it is necessary to have scaffolds with excellent biocompatibility to meet the requirements of nerve regeneration. Good biocompatibility facilitates cell adhesion, does not cause inflammation, provides a good microenvironment for cell growth, and can be used safely within the human body. In addition, appropriate biocompatibility can facilitate axonal growth by incorporating biomolecules such as full-length proteins or shorter peptide chains that mimic the native extracellular matrix [33].
Biodegradability
The ideal biological scaffold should have a good affinity with tissues during the process of organism degradation. To provide space for nerve regeneration after injury, avoiding additional harm caused by the secondary procedure of scaffold removal [20]. In addition, the biodegradation rate should align with the nerve regeneration rate, which can be artificially regulated or self-regulated to avoid scaffold degradation too fast or too slow to provide adequate supporting effects for SCI.
Physical property
The biological scaffold material should have mechanical properties that are compatible with spinal cord lesions: adequate strength, hardness, and elasticity [34]. A good fibrin scaffold not only promotes axonal regeneration but also withstands the forces generated during spinal movement and the surrounding muscle tissues, so as to provide adequate protection for spinal cord regeneration. Ideally, SCI biomaterials can support axon growth with appropriate stiffness and provide space for axons to pass through or enter the scaffold.
Three-dimensional solid structure
A good fibrin scaffold can promote wound healing by establishing a three-dimensional spatial architecture and providing enough space for stem cells to adsorb on the scaffold surface. In addition, the three-dimensional porous structure can help cells interact by simulating the extracellular matrix, which is important for cell survival and growth [35].
The role of fibrin scaffolds in SCI
Creating a microenvironment for cell regeneration
Fibrin provides a loose microenvironment for cell adhesion and axonal regeneration by adhering to other embedded proteins. Fibrin-based scaffold materials have significant potential as matrices for the delivery of growth factors or cell therapy after SCI. In particular, studies have shown that fibrin scaffolds can be used as carriers of neurotrophic factors to support the regeneration of injured nerves [36]. In addition, the axial holes, channels, and arranged fibers are conducive to controlling the growth direction of the nerve structures [37]. The porosity of a well-designed fibrin scaffold is beneficial for enhanced cell adhesion, which is critical for providing a larger bridge distance.
Providing a platform for cell attachment
Fibrin is a natural nano scaffold that provides a platform for stem cell transplantation, promoting cellular activity and extracellular matrix deposition [38]. Due to its high biocompatibility, fibrin is used to support stem cell transplantation for attachment and growth to promote nerve regeneration. Previous studies have shown that fibrin scaffolds are widely used to support the differentiation of embryonic stem cell-derived NPCs into neurons and oligodendrocytes, as well as the development of an effective cell delivery platform for neurons derived from pluripotent stem cells [39]. Willerth et al. [40] confirmed through research that fibrin scaffold can be used as a platform for neural tissue engineering to treat SCI. Other studies have shown that mesenchymal stem cells (MSCs) cultured in fibrin glue exhibit robust viability and enhanced differentiation potential, promoting MSCs to differentiate into neurons [41, 42].
Fibrin scaffold combined with stem cell trans- plantation for spinal cord repair
Although various medical technologies have changed with each passing day, there is no effective way to solve the problem of nerve regeneration. Stem cell transplantation have shown the potential of neuroprotection and nerve regeneration in SCI, with various targets and responses to stimuli, such as regulating inflammatory response, providing nutritional support, and improving plasticity [43]. The therapeutic principles of stem cells for SCI include replacement of damaged neurons and glial cells, secretion of trophic factors, inhibition of glial scar formation, and promotion of axon regeneration. Among these, it is more important that stem cell transplantation can prevent or replace damaged glial cells, especially oligodendrocytes, which can promote the remyelination of surviving axons [44] (Figure 1B & C). The fibrin scaffold technology can provide support and guide the growth of stem cell-derived axons, provide protection for new axons, avoid scar tissue invasion, reduce the apoptosis of transplanted stem cells, and improve the survival rate of transplanted cells. The following are some of the hot research topics in recent years on the combination of stem cells and SCI (Table 1).
Table 1
Fibrin scaffold combined with different types of stem cells for treatment of SCI.
| Stem cell types | Experimental methods | Outcome | Ref. |
|---|---|---|---|
| ESC-derived NPCs | NPCs + fibrin scaffold containing HBDS, NT-3, and PDGF. | NPCs↑ and neuron↑ | [45] |
| ESCs | Retinoic acid was added to EBs to induce mouse ESCs to become NPCs and implanted into fibrin scaffolds of different concentrations. | Optimal concentrations for scaffold polymerization were 10 mg/mL of fibrinogen and 2 NIH units/mL of thrombin. The optimal aprotinin concentration was determined to be 50 μg/mL for dissociated EBs (2D) and 5 μg/mL for intact EBs in 3D fibrin scaffolds. | [40] |
| iPSCs | An 8-day (4-/4+) protocol using soluble retinoic acid in the last 4 days and a 6-day (2-/4+) protocol using soluble retinoic acid and the small molecule sonic hedgehog agonist purmorphamine. | In iPSCs and ESCs, the proportion of neurons generated by EBs generated by 2-/4+ protocol is higher. | [46] |
| BM-MSCs | BM-MSCs were affixed with fibrin glue and injected inside or around the graft. | Repaired rat sciatic nerve. | [42] |
| BM-MSCs | Female adult rats were subjected to SCI. 60 days after lesion, rats were randomly distributed in four groups: (1) Rats immunized with complete Freund’s adjuvant + PBS (vehicle; PBS-I); (2) Rats with SR + FGM-MSCs; (3) Rats with SR + INDP + FGM-MSCs; (4) Rats only with INDP. | Treatment with INDP alone significantly increased motor recovery, anti-inflammatory cytokines, regeneration-associated molecules, axonal regeneration, and neurogenesis. | [45] |
| AD-MSCs | The derived progenitors, tagged with fluorescent tracker dye were delivered in rat T10 contusion SCI using fibrin hydrogel. | Fibrin niche aided stable differentiation of rat ADMSCs into neural progenitors. | [48] |
| NSCs | NSCs were implanted into fibrin matrix containing growth factor cocktails. | The injured spinal cord extended a large number of axons and formed neuronal relay, and the electrophysiological function of the rats recovered at the same time. | [26] |
| NSCs | Fresh NSCs were isolated from transgenic Fischer 344 rat embryos expressing GFP and embedded in fibrin matrix containing growth factors. | The graft completely filled the lesion cavity and differentiated into two types of neurons (axons extended very far from the host spinal cord) and glial cells. | [49] |
Embryonic stem cells
Embryonic stem cells (ESCs) can differentiate into a variety of neuronal cell types, which has great potential as a cell replacement therapy after SCI. It has been shown that an appropriate fibrin scaffold can enhance the activity of ESC-derived NPCs [50, 51]. Johnson et al. [45] embedded ESC-derived NPCs containing growth factor and heparin-binding delivery system (HBDS) and found that the combination of neurotrophin-3 (NT-3), plateletderived growth factor (PDGF) and fibrin scaffold could increase the number of NPCs at the site of SCI. The results prove that the application of fibrin scaffold can help to increase the survival and differentiation of ESC-derived NPCs at the injured site, and this discovery will help to increase the feasibility of fibrin scaffold combined with stem cell transplantation in the treatment of SCI. In addition, Willerth et al. [40] experimentally determined the culture conditions suitable for proliferation and differentiation of ESCs in fibrin scaffold. The optimal concentration for fibrin scaffold polymerization is 10 mg/mL of fibrinogen and 2 NIH units/mL of thrombin. After 14 days of continuous culture in the scaffold, ESCs were found to differentiate into neurons and astrocytes by immunohistochemistry. Therefore, there is a certain possibility for the treatment of spinal cord injuries in the elderly population through the combination of ESCs and fibrin scaffolds.
Induced pluripotent stem cells
Induced pluripotent stem cells (iPSCs) reprogram terminally differentiated somatic cells into pluripotent stem cells by introducing specific transcription factors into adult somatic cells [52, 53]. After reprogramming under specific conditions, the differentiated somatic cells returned to the totipotent state. Montgomery et al. [46] designed two systems to investigate whether iPSCs, when combination with fibrin scaffold, could increase the number of iPSCs differentiated into neural cells. The results confirmed that the differentiation ability of iPSCs on the fibrin scaffold platform was improved, and the promotion of neurons generated from murine iPSC-derived EBs seeded in fiber could be maximized using the 2-/4+ differentiation protocol. Bahareh et al. [54] discovered that fibronectin hydrogels can enhance cell viability and promote the differentiation of iPSCs into pre-oligodendrocytes. These experiments verified that 3D fibrin can improve the survival rate of transplanted stem cells and the degree of transformation into neural cells. At the same time, it provides ideas and references for combining stem cell transplantation with fibrin scaffold for the treatment of SCI in aging society.
Mesenchymal stem cells
The combination of MSCs and a fibrin scaffold can promote the migration of mesenchymal cells across the blood-brain barrier in rats, facilitate the reconstruction of the neural glial cell pool, and induce differentiation into neuron-like cells and oligodendrocyte-like cells [38, 55]. The most commonly used MSCs in combination with fibrin for treating SCI are bone marrow mesenchymal stem cells (BM-MSCs) and adipose-derived mesenchymal stem cells (AD-MSCs). MSCs promote angiogenesis by expressing angiogenic factors, such as vascular endothelial growth factor (VEGF) [56]. In addition, MSCs can be used to promote axonal regeneration and myelination of the myelin sheath in nervous system injury, which is beneficial for nerve regeneration [42, 57, 58]. García Elisa et al. [59] observed mechanical retraction, increase of axonal fibers and recovery of motor and sensory function in rats after implantation of fibrin scaffold and BM-MSCs into injured spinal cord. Zhang et al. [60] demonstrated that the combined use of a fibrous scaffold and BM-MSCs significantly improved motor function in elderly rats compared to the use of the fibrous scaffold or BM-MSCs alone. Mukhamedshina et al. [61] investigated the effect of the combination of AD-MSCs and fibrin matrix on the post-traumatic response of the spinal cord in rats. The experiment showed that the application of AD-MSCs reduced the expression of astrocytes in the SCI area, and the combination of AD-MSCs and fibrin matrix significantly increased the expression of platelet-derived growth factor receptor (PDGFR) and HSPA1b mRNA, while decreasing the expression of ionized calcium-binding adapter molecule 1 in the central canal. Liu et al. [62] randomly divided the rat model of SCI into four groups: control group (laminectomy group), SCI group (laminectomy + spinal cord transection group), fibrin group (fibrin transplantation immediately after SCI), fibrin cell group [fibrin scaffold containing ectodermal mesenchymal stem cells (EM-SCs) implanted after SCI]. In comparison, it has been proven that the combination of ectodermal mesenchymal stem cells and fibrin scaffold in the treatment of SCI in rats is superior to the use of fibrin scaffold alone in terms of cell apoptosis rate, number of nerve fibers, myelin sheath thickness, and motor score. In the treatment of spinal cord injury in middle-aged and elderly patients, the combined use of acidic fibroblast growth factor (aFGF) secreted by MSCs and fibrin glue gel may help promote moderate neural regeneration [63, 64]. In addition, a large number of experiments support the conclusion that the fibrin niche contributes to the stable differentiation of rat MSCs into neural progenitor cells and promotes nerve tissue regeneration [47, 48, 65].
Neural stem cells
Neural stem cells (NSCs) are a group of cells that possess the ability to self-renew and differentiate into neurons and various types of glial cells. The transplanted neural stem cells replace the injured neurons and glial cells through renewal, thus reconnecting the injured spinal cord. Lu et al. [26] implanted NSCs into the fibrin matrix containing the growth factor cocktail, and found that a large number of axons extended in the injured spinal cord and formed neuronal relay, which improved the electrophysiological function of rats. Then, Lu et al. [49] separated fresh NSCs from transgenic Fischer 344 rat embryos expressing green fluorescent protein (GFP) and embedded them in fibrin matrix containing growth factors. The results showed that the graft completely filled the lesion cavity and differentiated into two types of neurons (the axons extended very far from the host spinal cord) and glial cells. Subsequently, Robinson et al. [66] experimentally verified the conclusions by Lu et al. [49]. Self-assembling peptide nanofiber scaffolds (SAPNS), which possess a fine three-dimensional structure and cell compatibility, can induce the differentiation of NSCs into neurons in vitro and promote axonal regeneration and improve hind limb motor function when transplanted in vivo [67]. Similarly, Arulmoli et al. [68] reported a novel composite scaffold composed of fibrin, hyaluronic acid, and laminin that can support the function of human neural stem/progenitor cells (HNSPCs). This composite biomaterial scaffold has physical properties suitable for HNSPCs and the central nervous system, supports the proliferation and differentiation of human neural stem/progenitor cells, and attenuates the rapid cell-mediated scaffold degradation. This has set a benchmark for the treatment of central nervous system injuries with biomaterials.
Summary and outlook
In this review, we have briefly discussed different types of stem cell transplantation combined with fibrin scaffold for the
treatment of SCI. SCI is a devastating neurological injury, and there is no single treatment that can completely restore the
injured spinal cord structure and function. Currently, the focus of SCI research is on stem cell transplantation and tissue
engineering scaffolds, but each has its own limitations. It is difficult to control the direction and amount of differentiation
of stem cells when they are transplanted into the injured spinal cord alone, and it is difficult to ensure the healthy survival of
transplanted stem cells in a poor microenvironment. Therefore, the use of tissue engineering scaffold technology can provide
support and guidance for the newborn axons, and at the same time can avoid the characteristics of the newborn axons being invaded
by scar tissue. It is a very potential research direction to combine the two technologies in the treatment of SCI.
However, at present, our research on the combination of fibrin scaffold and stem cell transplantation is still in the early stages
of exploration, and there are numerous directions that warrant further worthy of exploration and development. Therefore, the
following is our outlook for the future of this topic. First, we need to search for more types of stem cells and compare their
ability to differentiate into neurons to find the most suitable type for transplantation. Second, in the future research, we can
focus on the morphology and physical properties of the fibrin scaffold. Update the existing fibrin scaffold technology, improve
the mechanical properties of fibrin scaffold, and provide the best transplantation site for stem cells to protect them for better
proliferation and differentiation. Third, in the future, we can broaden our perspective and combine fibrin scaffold with stem cell
transplantation and growth factors for research. The advantages of different substances should be fully exploited to better reduce
neuronal damage after SCI, promote axon growth and rebuild the damaged spinal cord tissue.
Conclusions
In a word, for SCI, especially for elderly SCI, the current clinical treatment effect is not satisfactory. Based on the understanding of the pathological changes of SCI, with the deepening of research on stem cell transplantation combined with fibrin scaffold, this treatment strategy may be a promising choice for the regenerative treatment of SCI patients.
Declarations
Author contributions
TJ and ZC jointly wrote the manuscript and produced and revised pictures and tables. YH participated in critical revision of the manuscript for intellectual content. XT and YL sorted out and screened the relevant literatures. HY designed the outline and revised the paper. All authors have read and approved the final version of this manuscript.
Conflicts of interest
The authors declare that they have no conflicts of interest related to this work.
Acknowledgments
The authors thank all the participants for sharing their perspectives in this study. We would also like to thank Prof. Yongxiong He from the Second Affiliated Hospital of Hainan Medical University for his guidance. We also thank our editor and reviewers for their untiring help and constructive comments. This work was supported by the National Natural Science Foundation of China [grant number 82060398].
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
References
1. Chay W, & Kirshblum S. Predicting outcomes after spinal cord injury. Phys Med Rehabil Clin N Am, 2020, 31(3): 331-343. [Crossref]
2. Hiremath SV, Karmarkar AM, Kumar A, Coffman DL, & Marino RJ. Factors associated with post-acute functional status and discharge dispositions in individuals with spinal cord injury. J Spinal Cord Med, 2022, 45(1): 126-136.[Crossref]
3. Jiang T, & He Y. Recent advances in the role of nuclear factor erythroid-2-related factor 2 in spinal cord injury: regulatory mechanisms and therapeutic options. Front Aging Neurosci, 2022, 14: 851257. [Crossref]
4. Liu X, Zhang Y, Wang Y, & Qian T. Inflammatory response to spinal cord injury and its treatment. World Neurosurg, 2021, 155: 19-31. [Crossref]
5. Tran AP, Warren PM, & Silver J. The biology of regeneration failure and success after spinal cord injury. Physiol Rev, 2018, 98(2): 881-917. [Crossref]
6. Pang QM, Chen SY, Xu QJ, Fu SP, Yang YC, Zou WH, et al. Neuroinflammation and scarring after spinal cord injury: Therapeutic Roles of MSCs on Inflammation and Glial Scar. Front Immunol, 2021, 12: 751021. [Crossref]
7. Khaing ZZ, Thomas RC, Geissler SA, & Schmidt CE. Advanced biomaterials for repairing the nervous system: what can hydrogels do for the brain? Materials Today, 2014, 17(7): 332-340. [Crossref]
8. Papastefanaki F, & Matsas R. From demyelination to remyelination: the road toward therapies for spinal cord injury. Glia, 2015, 63(7): 1101-1125. [Crossref]
9. Tian DS, Dong Q, Pan DJ, He Y, Yu ZY, Xie MJ, et al. Attenuation of astrogliosis by suppressing of microglial proliferation with the cell cycle inhibitor olomoucine in rat spinal cord injury model. Brain Res, 2007, 1154: 206- 214. [Crossref]
10. Zipser CM, Cragg JJ, Guest JD, Fehlings MG, Jutzeler CR, Anderson AJ, et al. Cell-based and stem-cell-based treatments for spinal cord injury: evidence from clinical trials. Lancet Neurol, 2022, 21(7): 659-670. [Crossref]
11. Mothe AJ, & Tator CH. Review of transplantation of neural stem/progenitor cells for spinal cord injury. Int J Dev Neurosci, 2013, 31(7): 701-713. [Crossref]
12. Coppé JP, Desprez PY, Krtolica A, & Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol, 2010, 5: 99-118. [Crossref]
13. Tchkonia T, Zhu Y, van Deursen J, Campisi J, & Kirkland JL. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest, 2013, 123(3): 966-972. [Crossref]
14. Takano M, Kawabata S, Shibata S, Yasuda A, Nori S, Tsuji O, et al. Enhanced functional recovery from spinal cord injury in aged mice after stem cell transplantation through HGF induction. Stem Cell Reports, 2017, 8(3): 509-518. [Crossref]
15. Siegenthaler MM, Berchtold NC, Cotman CW, & Keirstead HS. Voluntary running attenuates age-related deficits following SCI. Exp Neurol, 2008, 210(1): 207-216. [Crossref]
16. Jaerve A, Kruse F, Malik K, Hartung HP, & Müller HW. Age-dependent modulation of cortical transcriptomes in spinal cord injury and repair. PLoS One, 2012, 7(12): e49812. [Crossref]
17. Hooshmand MJ, Galvan MD, Partida E, & Anderson AJ. Characterization of recovery, repair, and inflammatory processes following contusion spinal cord injury in old female rats: is age a limitation? Immun Ageing, 2014, 11: 15-25. [Crossref]
18. von Leden RE, Khayrullina G, Moritz KE, & Byrnes KR. Age exacerbates microglial activation, oxidative stress, inflammatory and NOX2 gene expression, and delays functional recovery in a middle-aged rodent model of spinal cord injury. J Neuroinflammation, 2017, 14(1): 161-171. [Crossref]
19. Ansorena E, De Berdt P, Ucakar B, Simón-Yarza T, Jacobs D, Schakman O, et al. Injectable alginate hydrogel loaded with GDNF promotes functional recovery in a hemisection model of spinal cord injury. Int J Pharm, 2013, 455(1-2): 148-158. [Crossref]
20. Shrestha B, Coykendall K, Li Y, Moon A, Priyadarshani P, & Yao L. Repair of injured spinal cord using biomaterial scaffolds and stem cells. Stem Cell Res Ther, 2014, 5(4): 91-101. [Crossref]
21. Itosaka H, Kuroda S, Shichinohe H, Yasuda H, Yano S, Kamei S, et al. Fibrin matrix provides a suitable scaffold for bone marrow stromal cells transplanted into injured spinal cord: a novel material for CNS tissue engineering. Neuropathology, 2009, 29(3): 248-257. [Crossref]
22. Domingues MM, Carvalho FA, & Santos NC. Nanomechanics of blood clot and thrombus formation. Annu Rev Biophys, 2022, 51: 201-221. [Crossref]
23. de la Puente P, & Ludeña D. Cell culture in autologous fibrin scaffolds for applications in tissue engineering. Exp Cell Res, 2014, 322(1): 1-11. [Crossref]
24. Chen Q, Zhang Z, Liu J, He Q, Zhou Y, Shao G, et al. A fibrin matrix promotes the differentiation of EMSCs isolated from nasal respiratory mucosa to myelinating phenotypical Schwann-like cells. Mol Cells, 2015, 38(3): 221- 228. [Crossref]
25. King VR, Alovskaya A, Wei DY, Brown RA, & Priestley JV. The use of injectable forms of fibrin and fibronectin to support axonal ingrowth after spinal cord injury. Biomaterials, 2010, 31(15): 4447-4456. [Crossref]
26. Lu P, Wang Y, Graham L, McHale K, Gao M, Wu D, et al. Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell, 2012, 150(6): 1264-1273. [Crossref]
27. Park CH, & Woo KM. Fibrin-based biomaterial applications in tissue engineering and regenerative medicine. Adv Exp Med Biol, 2018, 1064: 253-261. [Crossref]
28. Yu Z, Li H, Xia P, Kong W, Chang Y, Fu C, et al. Application of fibrin-based hydrogels for nerve protection and regeneration after spinal cord injury. J Biol Eng, 2020, 14: 22-32. [Crossref]
29. Karimi A, Shojaei A, & Tehrani P. Mechanical properties of the human spinal cord under the compressive loading. J Chem Neuroanat, 2017, 86: 15-18. [Crossref]
30. Fehlings MG, Chen Y, Aarabi B, Ahmad F, Anderson KD, Dumont T, et al. A randomized controlled trial of local delivery of a Rho inhibitor (VX-210) in patients with acute traumatic cervical spinal cord injury. J Neurotrauma, 2021, 38(15): 2065-2072. [Crossref]
31. Schmidt CE, & Leach JB. Neural tissue engineering: strategies for repair and regeneration. Annu Rev Biomed Eng, 2003, 5: 293-347. [Crossref]
32. Tsai EC, Dalton PD, Shoichet MS, & Tator CH. Matrix inclusion within synthetic hydrogel guidance channels improves specific supraspinal and local axonal regeneration after complete spinal cord transection. Biomaterials, 2006, 27(3): 519-533. [Crossref]
33. Straley KS, Foo CW, & Heilshorn SC. Biomaterial design strategies for the treatment of spinal cord injuries. J Neurotrauma, 2010, 27(1): 1-19. [Crossref]
34. Zhang Q, Shi B, Ding J, Yan L, Thawani JP, Fu C, et al. Polymer scaffolds facilitate spinal cord injury repair. Acta Biomater, 2019, 88: 57-77. [Crossref]
35. Zamani F, Amani-Tehran M, Latifi M, Shokrgozar MA, & Zaminy A. Promotion of spinal cord axon regeneration by 3D nanofibrous core-sheath scaffolds. J Biomed Mater Res A, 2014, 102(2): 506-513. [Crossref]
36. Jeon O, Ryu SH, Chung JH, & Kim BS. Control of basic fibroblast growth factor release from fibrin gel with heparin and concentrations of fibrinogen and thrombin. J Control Release, 2005, 105(3): 249-259. [Crossref]
37. Madaghiele M, Sannino A, Yannas IV, & Spector M. Collagen-based matrices with axially oriented pores. J Biomed Mater Res A, 2008, 85(3): 757-767. [Crossref]
38. Blando S, Anchesi I, Mazzon E, & Gugliandolo A. Can a scaffold enriched with mesenchymal stem cells be a good treatment for spinal cord injury? Int J Mol Sci, 2022, 23(14): 7545-7555. [Crossref]
39. Willerth SM, Rader A, & Sakiyama-Elbert SE. The effect of controlled growth factor delivery on embryonic stem cell differentiation inside fibrin scaffolds. Stem Cell Res, 2008, 1(3): 205-218. [Crossref]
40. Willerth SM, Arendas KJ, Gottlieb DI, & Sakiyama-Elbert SE. Optimization of fibrin scaffolds for differentiation of murine embryonic stem cells into neural lineage cells. Biomaterials, 2006, 27(36): 5990-6003. [Crossref]
41. Yousefi F, Lavi Arab F, Nikkhah K, Amiri H, & Mahmoudi M. Novel approaches using mesenchymal stem cells for curing peripheral nerve injuries. Life Sci, 2019, 221: 99- 108. [Crossref]
42. Zhao Z, Wang Y, Peng J, Ren Z, Zhang L, Guo Q, et al. Improvement in nerve regeneration through a decellularized nerve graft by supplementation with bone marrow stromal cells in fibrin. Cell Transplant, 2014, 23(1): 97- 110. [Crossref]
43. Huang L, Fu C, Xiong F, He C, & Wei Q. Stem cell therapy for spinal cord injury. Cell Transplant, 2021, 30: 963689721989266. [Crossref]
44. Muheremu A, Peng J, & Ao Q. Stem cell based therapies for spinal cord injury. Tissue Cell, 2016, 48(4): 328-333. [Crossref]
45. Johnson PJ, Tatara A, Shiu A, & Sakiyama-Elbert SE. Controlled release of neurotrophin-3 and platelet-derived growth factor from fibrin scaffolds containing neural progenitor cells enhances survival and differentiation into neurons in a subacute model of SCI. Cell Transplant, 2010, 19(1): 89-101. [Crossref]
46. Montgomery A, Wong A, Gabers N, & Willerth SM. Engineering personalized neural tissue by combining induced pluripotent stem cells with fibrin scaffolds. Biomater Sci, 2015, 3(2): 401-413. [Crossref]
47. Rodríguez-Barrera R, Flores-Romero A, Buzoianu-Anguiano V, Garcia E, Soria-Zavala K, Incontri-Abraham D, et al. Use of a combination strategy to improve morphological and functional recovery in rats with chronic spinal cord injury. Front Neurol, 2020, 11: 189-199. [Crossref]
48. Chandrababu K, Sreelatha HV, Sudhadevi T, Anil A, Arumugam S, & Krishnan LK. In vivo neural tissue engineering using adipose-derived mesenchymal stem cells and fibrin matrix. J Spinal Cord Med, 2023, 46(2): 262-276. [Crossref]
49. Lu P, Graham L, Wang Y, Wu D, & Tuszynski M. Promotion of survival and differentiation of neural stem cells with fibrin and growth factor cocktails after severe spinal cord injury. J Vis Exp, 2014, (89): e50641. [Crossref]
50. McCreedy DA, Wilems TS, Xu H, Butts JC, Brown CR, Smith AW, et al. Survival, differentiation, and migration of high-purity mouse embryonic stem cell-derived progenitor motor neurons in fibrin scaffolds after sub-acute spinal cord injury. Biomater Sci, 2014, 2(11): 1672-1682. [Crossref]
51. Willerth SM, Faxel TE, Gottlieb DI, & Sakiyama-Elbert SE. The effects of soluble growth factors on embryonic stem cell differentiation inside of fibrin scaffolds. Stem Cells, 2007, 25(9): 2235-2244. [Crossref]
52. Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell, 2007, 131(5): 861-872. [Crossref]
53. Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science, 2007, 318(5858): 1917-1920. [Crossref]
54. Nazari B, Kazemi M, Kamyab A, Nazari B, EbrahimiBarough S, Hadjighassem M, et al. Fibrin hydrogel as a scaffold for differentiation of induced pluripotent stem cells into oligodendrocytes. J Biomed Mater Res B Appl Biomater, 2020, 108(1): 192-200. [Crossref]
55. Mortazavi MM, Harmon OA, Adeeb N, Deep A, & Tubbs RS. Treatment of spinal cord injury: a review of engineering using neural and mesenchymal stem cells. Clin Anat, 2015, 28(1): 37-44. [Crossref]
56. Chun SY, Lim JO, Lee EH, Han MH, Ha YS, Lee JN, et al. Preparation and characterization of human adipose tissue-derived extracellular matrix, growth factors, and stem cells: a concise review. Tissue Eng Regen Med, 2019, 16(4): 385-393. [Crossref]
57. Gardin C, Vindigni V, Bressan E, Ferroni L, Nalesso E, Puppa AD, et al. Hyaluronan and fibrin biomaterial as scaffolds for neuronal differentiation of adult stem cells derived from adipose tissue and skin. Int J Mol Sci, 2011, 12(10): 6749-6764. [Crossref]
58. Wu X, Ren J, & Li J. Fibrin glue as the cell-delivery vehicle for mesenchymal stromal cells in regenerative medicine. Cytotherapy, 2012, 14(5): 555-562. [Crossref]
59. García E, Rodríguez-Barrera R, Buzoianu-Anguiano V, Flores-Romero A, Malagón-Axotla E, Guerrero-Godinez M, et al. Use of a combination strategy to improve neuroprotection and neuroregeneration in a rat model of acute spinal cord injury. Neural Regen Res, 2019, 14(6): 1060-1068. [Crossref]
60. Zhang D, Sun Y, & Liu W. Motor functional recovery efficacy of scaffolds with bone marrow stem cells in rat spinal cord injury: a Bayesian network meta-analysis. Spinal Cord, 2023, 61(2): 93-98. [Crossref]
61. Mukhamedshina YO, Akhmetzyanova ER, Kostennikov AA, Zakirova EY, Galieva LR, Garanina EE, et al. Adiposederived mesenchymal stem cell application combined with fibrin matrix promotes structural and functional recovery following spinal cord injury in rats. Front Pharmacol, 2018, 9: 343-353. [Crossref]
62. Liu J, Chen Q, Zhang Z, Zheng Y, Sun X, Cao X, et al. Fibrin scaffolds containing ectomesenchymal stem cells enhance behavioral and histological improvement in a rat model of spinal cord injury. Cells Tissues Organs, 2013, 198(1): 35-46. [Crossref]
63. Wu JC, Huang WC, Tsai YA, Chen YC, & Cheng H. Nerve repair using acidic fibroblast growth factor in human cervical spinal cord injury: a preliminary Phase I clinical study. J Neurosurg Spine, 2008, 8(3): 208-214. [Crossref]
64. Wu JC, Huang WC, Chen YC, Tu TH, Tsai YA, Huang SF, et al. Acidic fibroblast growth factor for repair of human spinal cord injury: a clinical trial. J Neurosurg Spine, 2011, 15(3): 216-227. [Crossref]
65. Ibarra A, Mendieta-Arbesú E, Suarez-Meade P, GarcíaVences E, Martiñón S, Rodriguez-Barrera R, et al. Motor recovery after chronic spinal cord transection in rats: a proof-of-concept study evaluating a combined strategy. CNS Neurol Disord Drug Targets, 2019, 18(1): 52-62. [Crossref]
66. Robinson J, & Lu P. Optimization of trophic support for neural stem cell grafts in sites of spinal cord injury. Exp Neurol, 2017, 291: 87-97. [Crossref]
67. Wan JM, Liu LL, Zhang JF, Lu JW, & Li Q. Promotion of neuronal regeneration by using self-polymerized dendritic polypeptide scaffold for spinal cord tissue engineering. J Mater Sci Mater Med, 2017, 29(1): 6-16. [Crossref]
68. Arulmoli J, Wright HJ, Phan DTT, Sheth U, Que RA, Botten GA, et al. Combination scaffolds of salmon fibrin, hyaluronic acid, and laminin for human neural stem cell and vascular tissue engineering. Acta Biomater, 2016, 43: 122-138. [Crossref]