Open Access | Case Report
This work is licensed under a Creative
Commons Attribution-ShareAlike 4.0 International License.
Laparoscopic nephrectomy with mini-incision kidney autotransplantation in severe ureteral strictures: report of three cases and review of the literature
* Urology Unit, Centro Salute Uomo, Via Palma
il Vecchio 4a, 24122 Bergamo, Italy.
Email: francesco_greco@ymail.com
Received: 20 June 2022 / Revised: 29 July 2022 / Accepted: 06 September 2022 / Published: 26 September 2022
DOI: 10.31491/UTJ.2022.09.002
Abstract
Severe and long ureteral injuries are difficult to be managed. In presence of a complex injury of the upper ureter, nephrectomy, bowel interposition, and kidney autotransplantation (KAT) are usually proposed. Kidney autotransplantation (KAT) represents a complex surgical procedure with a high risk of complications that could preserve renal function. We update our experience with renal autotransplantation for severe iatrogenic ureteral injuries. Three patients with complex ureteral injuries were referred for definitive management by KAT. Transperitoneal laparoscopic nephrectomy (LN) and open mini-incision KAT (mKAT) to the ipsilateral pelvis were attempted. After bench preparation of the graft, ureteral and vessel length and quality was adequate for autotransplantation in all cases. There were no intra- and postoperative complications and all grafts functioned immediately and at medium-term follow-up of 6 months. KAT gives excellent post-operative results without significant deterioration in renal function at medium-term follow-up. It represents a safe alternative method for the management of complex ureteric strictures when conventional surgical techniques have failed or are not suitable. Intensive collaboration with all transplant teams is crucial to ensure the high quality of the graft and to improve surgical and functional outcomes.
Keywords
Ureteral stricture, autotransplantation, kidney, surgery
Introduction
Severe and long ureteral injuries are difficult to be managed. In presence of a complex injury of the upper ureter, nephrectomy, bowel interposition, and kidney autotransplantation (KAT) are usually proposed. In 1962, Hardy [1] reported the first case report of a patient in which the right ureter, placed behind an aortic prosthesis 6 years earlier, was unwittingly severed during resection of a large aneurysmal homograft. The patient developed stenosis of the ureteroureteral anastomosis and underwent autotransplantation of the right kidney into the right iliac fossa. The renal vessels were anastomosed to the external iliac artery and vein and the ureter was implanted into the bladder. Surgery was successful with a normal postoperative graft function at renal scintigraphy and anterograde urography. Since then, KAT has been proposed as valid therapy to preserve kidneys with complex renovascular, ureteral, or malignant diseases [2]. Common indications for KAT are represented by complex lesions of renal vessels, high ureteral strictures which cannot be treated by an endoscopic approach, and high PADUA-score renal tumors, especially for imperative indications [2, 3]. Moreover, KAT could be also indicated, but with a lower incidence, for retroperitoneal fibrosis, and metabolic stone disease [2, 4, 5]. Even if the intra- and postoperative mortality rates after KAT are low (1.3%), postoperative morbidity is still clinically significant (46.2%) [2]. Since Fabrizio et al. [6] reported the first laparoscopic nephrectomy (LN) for KAT in 2000, this mini-invasive procedure with reduced surgical trauma for the patient has been proposed as the gold standard. In this study, we present our experience with LN and mini-incision KAT (mKAT) in the treatment of severe iatrogenic injuries of the upper ureter.
Case reports
Case 1
JW, a 37-year-old male presented with a chronic urinary infection. The patient has undergone a prophylactic total colectomy 10 years before for familial polyposis coli. Following surgery, the patient developed ureteral stricture bilaterally, that were managed by introducing ureteral double-J (DJ) stents bilaterally. The renal scintigraphy showed a severely reduced renal function over time, which finally resulted in 13% on the left side and 87 % on the right side. Physical examination was normal. Blood count, serum creatinine, and blood urea nitrogen (BUN) were normal. After placement of two percutaneous nephrectomies, the patient underwent an antegrade (APG) and retrograde ureteropyelography (UPG); both diagnostic procedures revealed bilateral hydroureteronephrosis with multiple right ureteral strictures (Figure 1).

Figure 1. Antegrade and retrograde ureteropyelography showing bilateral hydronephrosis with multiple right ureteral stenoses.
mKAT was planned for the definitive management of the ureteral stricture to spare the residual renal function. The patient underwent transperitoneal laparoscopic surgery with segmental ureterectomy and nephrectomy of the right side. The first surgical step was represented by the dissection of all intraperitoneal adherences due to the previous laparotomy. Afterward, the right kidney was prepared with a dissection of renal vessels. The renal vein was gently dissected up to the insertion into the vena cava, thus assuring an adequate length of the vessels. The renal vein was dissected first, followed by the renal artery, by a triple-row Endo-TA stapler (Multi fire Endo TA 30; Covidien), thus achieving longer perfusion of the kidney and reducing the warm ischemia time. Mini-incision KAT followed in the right iliac fossa with renal artery anastomosed to the right external iliac artery, renal vein to the right external iliac vein and the ureter was reimplanted by an extravesical and anti-reflux technique using a Lich-Gregoir technique [7]. No intra- and postoperative complications occurred. The operating time was 310 minutes with median vascular and ureteral anastomosis times of 19 and 12 min, respectively. Warm, cold, and rewarming ischemia time was 8, 100, and 24 min, respectively. Skin incision for mKAT was 6 cm and postoperative oral intake (POI) was started on day 1, with a VAS of 2. Hospital stay was 6 days and at discharge, VAS was 1. The serum creatinine improved from 243 µmol/l preoperatively to 187 µmol/L at discharge. Two months after mKAT, serum creatinine was 160 µmol/ l with normal vascular perfusion of the auto-graft at doppler sonography. At 2 years follow-up, mean serum creatinine of 190 µmol//L with good vascular perfusion of the auto transplanted renal unit at doppler sonography (Figure 2).

Figure 2. Duplex Ultrasound after kidney autotransplantation at 2-yr follow-up.
Case 2
M.D., a 26 years old male presented with a history of left pyelonephritis with severe hydronephrosis. The attempt to place a ureteral DJ stent failed for severe stenosis of the upper left ureter so a percutaneous nephrostomy was necessary. In the medical history, the patient underwent combined radio-chemotherapy and lumbar vertebral fixation for an Ewing’s sarcoma of the vertebral L-column (L 1-2). Physical examination was normal. APG showed left hydronephrosis determined by stricture of the whole ureter (Figure 3). Renal scintigraphy and computed tomography revealed a reduction of the renal function on the left side (41%) with a severe stricture of the left ureter in all its course (Figure 4).
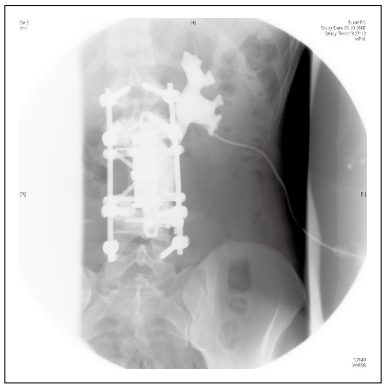
Figure 3. Antegrade ureteropyelography showing left hydronephrosis with long ureteral stricture.
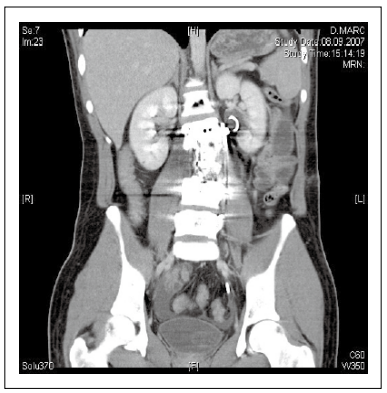
Figure 4. Computed tomography shows the left ureteral stenosis after vertebral fixation.
The patient underwent left LN and mKAT. The operating time was 360 min with median vascular and ureteral anastomosis times of 25 and 17 min, respectively. Warm, cold, and rewarming ischemia time was 18, 130, and 22 min, respectively. Skin incision for KAT was 6 cm and POI was started on day 1 with a VAS of 3. On the 1st postoperative day, the patient presented a fever up to 38.7 which was solved by antibiotics and paracetamol so he was discharged on the 7th postoperative day with a VAS of 1. At a follow-up of 19 months, mean serum creatinine was 120 µmol//L with normal vascular perfusion of the autotransplant renal unit at doppler sonography.
Case 3
RF, a 60 years old male presented with long ureteral proximal stricture after ureteroscopy, lithotripsy, and stone extraction. After the primary operation, the patient developed chronic urinary tract infections and arterial hypertension. The radiological diagnostic examinations showed long stenosis located in the upper and the middle portion of the left ureter (Figure 5) The renal scintigraphy showed a bilateral normal renal function but a reduced renal excretion function for the left kidney. Blood count, serum creatinine, and BUN were normal. Left LN and mKAT were undertaken for the management of the ureteral stricture to spare renal function and improve the quality of life. The operating time was 330 min with median vascular and ureteral anastomosis times of 21 and 14 min, respectively. Warm, cold, and rewarming ischemia time was 19, 90, and 25 min, respectively. No intra- and postoperative complications occurred. Skin incision for KAT was 6 cm and POI was started on day 1, with a VAS of 2. Hospital stay was 6 days and at discharge, VAS was 1. At 2 years follow-up, the serum creatinine was 109 µmol/L, and also in this case doppler sonography reported normal vascular perfusion of autotransplant renal unit.

Figure 5. Antegrade ureteropyelography via percutaneous nephrostomy showed proximal ureteral stenosis left.
Discussion
Severe ureteral injuries are rare, occurring in less than 4%
and 1% of penetrating and blunt traumas, respectively.
Ureteral injuries result from either iatrogenic or external
trauma. Iatrogenic ureteral injuries far outnumber traumatic injuries, and they usually happen after endourological procedures [8]. The improvements in equipment and
operator experience have subsequently lowered the rate
to a stable average of 7% (range, 0% to 28%). However,
most of these injuries are minor and managed by placing a
DJ stent. Furthermore, iatrogenic ureteral injuries can also occur after pelvic surgery, such as hysterectomy (54%),
colorectal surgery (14%), transabdominal urethropexy
(8%), and abdominal vascular surgery (6%) [9]. Most
ureteral injuries can be endoscopically managed, with a
combination of internal ureteral stenting and percutaneous
nephrostomy tube drainage [10]. However, upper ureteral
injuries are usually managed by ureteroureterostomy. In
presence of a complete avulsion of the ureter from the
renal pelvis or very proximal ureteral lesion, reimplantation of the ureter directly into the renal pelvis can be performed by spatulating the ureter and performing a watertight and tension-free anastomosis after placing a DJ stent.
Laparoscopic pyeloplasty has been reported [11-14] and
it is likely to become more widespread for the very high
ureteral lesion. Ileal interposition can be used in cases of
delayed ureteral repair, especially when a very long ureteral segment is damaged [15]. Ileum interposition should
be avoided in patients with previous intestinal surgery,
inflammatory intestinal diseases, and chronic renal insufficiency.
Moreover, a recent study has suggested an overall success
rate for ileum interposition at a mean follow-up of 4.4
years (1-16 years) of 83%, with 17% of patients requiring
subsequent major surgery (5 successful ureteral revision,
3 nephrectomies) and 24% of the patients experiencing a
major complication such as urinary fistula, surgical site
infection requiring open washout and ureteral obstruction
[16].
In conclusion, ileum interposition represents a valid surgical technique with similar efficacy to KAT (81–88%); the
choice between ileal interposition and KAT is often a matter of the surgeon’s preference.
Kidney autotransplantation (KAT) can be usually proposed in presence of a long ureteral stricture or as the final
solution after multiple failed attempts of repair such as
ureteroureterostomy. During KAT, the kidney is harvested
with maximal vessel length as in a typical live donor nephrectomy for allotransplantation, and the renal vessels
are anastomosed to the iliac vessels to re-establish renal
perfusion. A healthy segment of the proximal ureter is
anastomosed to the bladder. Alternatively, the ipsilateral
renal pelvis may be anastomosed directly to the bladder
[17].
Currently, laparoscopic nephrectomy followed by open
autotransplantation represents the gold standard for KAT
[6]. Minimally invasive surgery aims to provide effective
treatment of surgical diseases inside a body cavity while
decreasing access-related morbidity, postoperative pain,
and hospital stay, and enabling faster recovery, improved
cosmesis, and patients’ early return to work [18, 19]. To
save a mini-invasive approach, we performed a mini skin
incision of 6 cm for performing autotransplantation. All
procedures were performed by an experienced surgeon
(FG), without any intra-or postoperative complications
and all patients referred lower pain according to VAS
on the 1st POD. In all cases, there was a postoperative
recovery of renal function. Our results reflect the actual
literature on KAT. In 2017, Ruiz et al . analyzed indications, surgical technique, complications, and long-term
outcomes of KAT in 15 patients at a single institution.
Indications for KAT were represented by vascular anomalies in 8 cases and ureteral injury in 7. Laparoscopic
nephrectomy was performed in 2 cases (13.3%) and an
open approach was used in 13 (86.7%). The mean hospital
stay was 9.1 days. Postoperative complications rate was
46.7%: 6 minor (Clavien I-II) and 1 major (Clavien III).
After a mean follow-up of 73.1 months, 80% of the patients have a functioning graft. The authors could suggest
that KAT results be an effective treatment for complex
ureteral lesions and kidney vascular abnormalities, with
good functional results in the long term and low risk for
surgical complications [20].
Similar outcomes were reported by Tran et al . in 52 patients who underwent laparoscopic nephrectomy with
autotransplantation. The indications were represented by
ureteral strictures (41), renal tumors (7), nephroptosis
(1), chronic flank pain (1), renal artery aneurysm (1), and
renovascular hypertension (1). At a median follow-up of
73.5 months, the auto transplanted renal unit presented
a normal function in 90.3% of the patients. Even in this
study, laparoscopic nephrectomy with autotransplantation
represented an excellent long-term surgical option in experienced hands for complex ureteral and renal conditions
that necessitate the preservation of renal parenchyma [21].
KAT gives excellent post-operative results without significant deterioration in renal function at medium-term
follow-up. It represents a safe alternative method for the
management of complex ureteric strictures when conventional surgical techniques have failed or are not suitable.
Intensive collaboration with all transplant teams is crucial
to ensure the high quality of the graft and to improve surgical and functional outcomes.
Declarations
Authors’ contributions
Made substantial contributions
to the conception and design of the study and performed
data analysis and interpretation: Francesco Greco.
Performed data acquisition, as well as providing administrative, technical, and material support: Antonino Inferrera, Luigi Domanico, Oreste Risi, and Paolo Fornara
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
Francesco Greco is a member of the Editorial Board of Uro-Technology Journal. The author declares no conflict of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
References
1. Hardy JD. High ureteral injuries. Management by autotransplantation of the kidney. JAMA, 1963, 184: 97-101. [Crossref]
2. Decaestecker K, Van Parys B, Van Besien J, Doumerc N, Desender L, Randon C, et al. Robot-assisted Kidney Autotransplantation: A Minimally Invasive Way to Salvage Kidneys. Eur Urol Focus, 2018, 4(2): 198-205. [Crossref]
3. Alameddine M, Moghadamyeghaneh Z, Yusufali A, Collazo AM, Jue JS, Zheng I, et al. Kidney Autotransplantation: Between the Past and the Future. Curr Urol Rep, 2018, 19(3): 7. [Crossref]
4. Cowan NG, Banerji JS, Johnston RB, Duty BD, Bakken B, Hedges JC, et al. Renal Autotransplantation: 27-Year Experience at 2 Institutions. J Urol, 2015, 194(5): 1357- 1361. [Crossref]
5. Azhar B, Patel S, Chadha P, & Hakim N. Indications for renal autotransplant: an overview. Exp Clin Transplant, 2015, 13(2): 109-114.
6. Fabrizio MD, Kavoussi LR, Jackman S, Chan DY, Tseng E, & Ratner LE. Laparoscopic nephrectomy for autotransplantation. Urology, 2000, 55(1): 145. [Crossref]
7. Kayler L, Kang D, Molmenti E, & Howard R. Kidney transplant ureteroneocystostomy techniques and complications: review of the literature. Transplant Proc, 2010, 42(5): 1413-1420. [Crossref]
8. Kaufman JJ. Ureteral injury from ureteroscopic stone manipulation. Urology, 1984, 23(3): 267-269.
9. St Lezin MA, & Stoller ML. Surgical ureteral injuries. Urology, 1991, 38(6): 497-506. [Crossref]
10. Selzman AA, & Spirnak JP. Iatrogenic ureteral injuries: a 20-year experience in treating 165 injuries. J Urol, 1996, 155(3): 878-881. [Crossref]
11. Kavoussi LR, & Peters CA. Laparoscopic pyeloplasty. J Urol, 1993, 150(6): 1891-1894. [Crossref]
12. Schuessler WW, Grune MT, Tecuanhuey LV, & Preminger GM. Laparoscopic dismembered pyeloplasty. J Urol, 1993, 150(6): 1795-1799. [Crossref]
13. Wagner S, Greco F, Inferrera A, Hoda MR, Kawan F, Hamza A, et al. Laparoscopic dismembered pyeloplasty: technique and results in 105 patients. World J Urol, 2010, 28(5): 615-618. [Crossref]
14. Bodie B, Novick AC, Rose M, & Straffon RA. Long-term results with renal autotransplantation for ureteral replacement. J Urol, 1986, 136(6): 1187-1189. [Crossref]
15. Boxer RJ. Reconstruction of the male external genitalia. Surg Gynecol Obstet, 1975, 141(6): 939-944.
16. Launer BM, Redger KD, Koslov DS, Sax-Bolder AN, Higuchi TT, Windsperger AP, et al. Long-term Follow Up of Ileal Ureteral Replacement for Complex Ureteral Strictures: Single Institution Study. Urology, 2021, 157: 257- 262. [Crossref]
17. Greco F, Alba S, Fornara P, & Mirone V. Renal transplantation: technical aspects, diagnosis and management of early and late urological complications. Panminerva Med, 2016, 58(4): 294-303.
18. Greco F, Hoda MR, Wagner S, Reichelt O, Inferrera A, Fischer K, et al. Adipocytokine: a new family of inflammatory and immunologic markers of invasiveness in major urologic surgery. Eur Urol, 2010, 58(5): 781-787. [Crossref]
19. Greco F, Veneziano D, Wagner S, Kawan F, Mohammed N, Hoda MR, et al. Laparoendoscopic single-site radical nephrectomy for renal cancer: technique and surgical outcomes. Eur Urol, 2012, 62(1): 168-174. [Crossref]
20. Ruiz M, Hevia V, Fabuel JJ, Fernández AA, Gómez V, & Burgos FJ. Kidney autotransplantation: long-term outcomes and complications. Experience in a tertiary hospital and literature review. Int Urol Nephrol, 2017, 49(11): 1929-1935. [Crossref]
21. Tran G, Ramaswamy K, Chi T, Meng M, Freise C, & Stoller ML. Laparoscopic Nephrectomy with Autotransplantation: Safety, Efficacy and Long-Term Durability. J Urol, 2015, 194(3): 738-743. [Crossref]